The scourge of PPH in Nigeria.pptx
- 1. The scourge of post partum haemorrhage in NIGERIA BY DR DUUM NWACHUKWU MBBS, FWACS,FMCOG, DMAS
- 2. INTRODUCTION ŌĆó Postpartum haemorrhage (PPH) is a major risk for mothers & newborns in Nigeria. Limited access to quality healthcare services and inadequate prenatal care contributes to the high incidence of this life- threatening condition. ŌĆó Postpartum haemorrhage is excessive bleeding following the birth of a baby and is a leading cause of maternal morbidity and mortality in Nigeria.
- 3. DEFINATION ŌĆó It is one of the leading causes of maternal mortality worldwide, including in Nigeria. ŌĆó Postpartum haemorrhage is defined as blood loss of more than 500 mL following a vaginal delivery or more than 1000 mL following cesarean delivery. A loss of these amounts within 24 hours of delivery is termed early or primary PPH, whereas such losses are termed late or secondary PPH if they occur 24 hours after delivery. ŌĆó
- 4. PROBLEMS WITH THIS DEFINITION ŌĆó The definition of PPH is somewhat arbitrary and problematic. Estimates of blood loss at delivery are subjective and generally inaccurate. Studies have suggested that caregivers consistently underestimate actual blood loss. Another proposal suggests using a 10% fall in hematocrit value to define PPH, but this change is dependent on the timing of the test
- 5. PROBLEMS WITH THIS DEFINITION(cont) ŌĆó Another consideration is the differing capacities of individual patients to cope with blood loss. A healthy woman has a 30-50% increase in blood volume in a normal singleton pregnancy and is much more tolerant of blood loss than a woman who has preexisting anaemia, an underlying cardiac condition, or a volume-contracted condition secondary to dehydration or preeclampsia. ŌĆó For these reasons, PPH should be diagnosed with any amount of blood loss that threatens the hemodynamic stability of the woman.
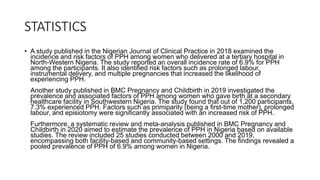
- 6. STATISTICS ŌĆó A study published in the Nigerian Journal of Clinical Practice in 2018 examined the incidence and risk factors of PPH among women who delivered at a tertiary hospital in North-Western Nigeria. The study reported an overall incidence rate of 6.9% for PPH among the participants. It also identified risk factors such as prolonged labour, instrumental delivery, and multiple pregnancies that increased the likelihood of experiencing PPH. Another study published in BMC Pregnancy and Childbirth in 2019 investigated the prevalence and associated factors of PPH among women who gave birth at a secondary healthcare facility in Southwestern Nigeria. The study found that out of 1,200 participants, 7.3% experienced PPH. Factors such as primiparity (being a first-time mother), prolonged labour, and episiotomy were significantly associated with an increased risk of PPH. Furthermore, a systematic review and meta-analysis published in BMC Pregnancy and Childbirth in 2020 aimed to estimate the prevalence of PPH in Nigeria based on available studies. The review included 25 studies conducted between 2000 and 2019, encompassing both facility-based and community-based settings. The findings revealed a pooled prevalence of PPH of 6.9% among women in Nigeria.
- 7. The Devastating Impacts of Postpartum Hemorrhage ŌĆó Mother: PPH can lead to maternal mortality, disability, depression, and an inability to breastfeed or care for her infant. ŌĆó Economics Impact: PPH can lead to increased healthcare costs, decreased productivity and increased poverty in affected families.
- 8. The Road to Saving Lives ŌĆó Skilled care during childbirth: 45% ŌĆó Nigeria has one of the highest maternal mortality rates in the world, but with crucial investments in healthcare infrastructure and additional medical resources, this problem can be prevented, and lives can be saved.
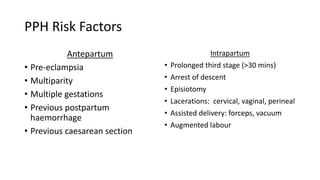
- 9. PPH Risk Factors Antepartum ŌĆó Pre-eclampsia ŌĆó Multiparity ŌĆó Multiple gestations ŌĆó Previous postpartum haemorrhage ŌĆó Previous caesarean section Intrapartum ŌĆó Prolonged third stage (>30 mins) ŌĆó Arrest of descent ŌĆó Episiotomy ŌĆó Lacerations: cervical, vaginal, perineal ŌĆó Assisted delivery: forceps, vacuum ŌĆó Augmented labour
- 10. Active management of third stage of labour (AMTSL) (AMTSL) is the key to reducing the risk of the complications ŌĆó As soon as the baby is delivered, put it on the motherŌĆÖs abdomen in skin-to-skin contact with her. Cover them with a blanket. ŌĆó Clamp the babyŌĆÖs umbilical cord at two sites and cut it in between. ŌĆó Check the uterus for the presence of a second baby. ŌĆó In less than one minute, administer a uterotonic drug (a hormone-like chemical that makes the uterus contract more powerfully). ŌĆó Apply controlled cord traction. ŌĆó After delivery of the placenta, immediately start massaging the uterus. ŌĆó Examine the placenta to make sure it is complete and none of it has been retained in the uterus. ŌĆó Examine the womanŌĆÖs vagina, perineum and external genitalia for lacerations and active bleeding.
- 11. Causes of PPH: The Four ŌĆ£TsŌĆØ ŌĆó Tone (70%) ŌĆó Trauma (20%) ŌĆó Tissue (10%) ŌĆó Thrombin (1%)
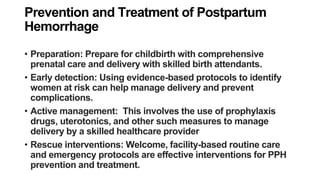
- 12. Prevention and Treatment of Postpartum Hemorrhage ŌĆó Preparation: Prepare for childbirth with comprehensive prenatal care and delivery with skilled birth attendants. ŌĆó Early detection: Using evidence-based protocols to identify women at risk can help manage delivery and prevent complications. ŌĆó Active management: This involves the use of prophylaxis drugs, uterotonics, and other such measures to manage delivery by a skilled healthcare provider ŌĆó Rescue interventions: Welcome, facility-based routine care and emergency protocols are effective interventions for PPH prevention and treatment.
- 13. PPH: Resuscitative Measures ŌĆó Call for help ŌĆó Airways, Breathing, Circulation ŌĆó Two large-bore IVs ŌĆó Oxygen ŌĆó Stat labs: type & cross, hb, coags ŌĆó Consider transfusion
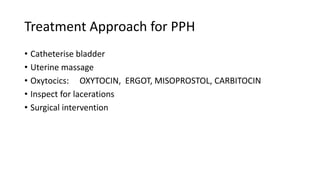
- 14. Treatment Approach for PPH ŌĆó Catheterise bladder ŌĆó Uterine massage ŌĆó Oxytocics: OXYTOCIN, ERGOT, MISOPROSTOL, CARBITOCIN ŌĆó Inspect for lacerations ŌĆó Surgical intervention
- 15. Access to Quality Healthcare Services 1 Infrastructure & Transportation ¤Ü¦ The government and private sector must invest in building and maintaining healthcare infrastructure and transportation systems to facilitate access to quality healthcare services. 2 Underserved Areas ¤ōŹ The lack of skilled birth attendants and emergency obstetric care facilities in remote areas has worsened the problem of postpartum hemorrhage in Nigeria. 3 Training & Capacity Building ¤Åŗ’ĖÅŌÖĆ’ĖÅ Continuous training and capacity building initiatives for healthcare providers can improve knowledge and skills needed to tackle postpartum hemorrhage effectively.
- 16. Comprehensive Prenatal Care Matters Importance of Regular Check- ups Regular check-ups during pregnancy can help detect potential complications and reduce the risk of postpartum hemorrhage. Nutrition & Proper Care Women need proper nutrition and prenatal care to stay healthy during pregnancy and prevent complications like postpartum hemorrhage. Antenatal Education Programs Antenatal education programs can raise awareness about the risks and warning signs of postpartum hemorrhage and empower women and their families to seek medical attention when needed.
- 17. Collaboration is Key 1 Government Intervention ’ĖÅ The government must create policies that prioritize maternal healthcare, including funding for healthcare infrastructure, training programs, and maternal health education initiatives. 2 Community Engagement ¤ī¤ Healthcare professionals, community leaders, and traditional birth attendants must cooperate to ensure that pregnant women have access to quality healthcare and that cultural beliefs do not hamper medical intervention. 3 Training & Capacity Building ¤ōÜ Training programs for traditional birth attendants can equip them with the skills to recognize and manage postpartum hemorrhage. Healthcare professionals also need continuous training to update their knowledge and skills.
- 18. The Importance of Prompt Medical Attention Rising to the Challenge ¤Æ¬ Women and families must recognize the warning signs of postpartum hemorrhage, such as excessive bleeding, and seek immediate medical attention. Overcoming Cultural Barriers ¤īŹ Cultural beliefs and practices that hinder prompt medical intervention must be addressed through culturally sensitive education and outreach programs. Advancing Technology & Innovation ¤īÉ Advances in technology and innovation must be leveraged to improve the diagnosis, prevention, and treatment of postpartum hemorrhage.
- 19. Improving Maternal Health Outcomes A Shared Responsibility Improving maternal health outcomes in Nigeria requires collaborative efforts between the government, healthcare professionals, community leaders, and traditional birth attendants. Access to Family Planning Services Improving access to family planning services can reduce the incidence of postpartum hemorrhage by spacing pregnancies and allowing women to plan their families. Early Pregnancy Testing & Care Early and effective pregnancy testing and care can reduce the risk of complications during childbirth and postpartum hemorrhage.
- 20. Making Progress Together 1 Data Collection & Reporting ¤ōØ The collection and analysis of data on maternal health outcomes can help to understand and address the drivers of postpartum hemorrhage in Nigeria. 2 Advocacy & Awareness ¤ōŻ Advocacy and awareness campaigns are crucial to mobilizing resources and public support to address the problem of postpartum hemorrhage in Nigeria. 3 Research & Innovation ¤ö¼ Research and innovation can lead to new interventions and approaches that can improve maternal health outcomes and prevent postpartum hemorrhage.
- 21. Empowering Women & Families 1 Maternal Health Education ¤Äō Providing education and information to women and families about maternal health and postpartum hemorrhage can empower them to make informed decisions and take action when needed. 2 Maternal Healthcare Services ¤Ü║ Ensuring access to quality maternal healthcare services, including skilled birth attendants, emergency obstetric care, and postpartum follow-up care, can improve maternal health outcomes in Nigeria. 3 Community Support ’ĖÅ Community support can be mobilized to help pregnant women access healthcare services and promote positive maternal health behaviors, leading to better outcomes for mothers and newborns.
- 22. Investment in Maternal Health Governments & Organizations ’ĖÅ Governments, organizations, and other stakeholders must invest in maternal healthcare to achieve better health outcomes in Nigeria. Family Support ’ĖÅ Family support is crucial to ensuring that pregnant women have access to the care and resources they need to prevent and manage postpartum hemorrhage. Advances in Healthcare Technology ¤ÜĆ Advances in healthcare technology, such as telemedicine and remote monitoring, can improve access to quality maternal healthcare services, particularly in remote areas.
- 23. The Way Forward 1 Collaboration & Partnership ’ĖÅ Collaborative partnerships between the government, healthcare professionals, traditional birth attendants, community leaders, and organizations can help to prevent postpartum hemorrhage and improve maternal health outcomes in Nigeria. 2 Empowerment & Education ¤ōÜ Empowering women and families through education and awareness can enable them to seek prompt medical attention and prevent postpartum hemorrhage. 3 Investment & Innovation ¤öÄ Investments in infrastructure, training, and innovation can help to overcome barriers and improve maternal health outcomes in Nigeria.
- 24. CONCLUSION ŌĆó EDUCATION ŌĆó AND ŌĆó EMPOWERMENT ŌĆó OF ŌĆó WOMEN AND COMMUNITY
- 26. BIBLIOGRAPHY ŌĆó Shittu O.S, Otubu JAM, postpartum Haemorrhage in Agboola A (ED). Textbook of obstetrics and gynaecology for medical students 2nd edition. Heinemann Educational books (Nig) Plc 2006: 481-488. ŌĆó Koh E, Devendra K, Tan L K. B-Lynch suture for the treatment of uterine atony. Singapore Med J 2009; 50(7): 693-697. ŌĆó Anderson JM, Etches Duncan. Prevention a n d ma n a g eme n t o f P o st p a rt um Haemorrhage. Am Fam Physician 2007; 75: 875-882. ŌĆó WHO. Guidelines for the Prevention of Postpartum Haemorrhage. Geneva: World Health Organization. 2007. ŌĆó Ajenifuja KO, Adepiti CA, Ogunniyi SO. Postpartum Haemorrhage in a Teaching Hospital: a 5-year experience. Afr Health Sci; 2010 10: 71-74.
- 27. ŌĆó Oladapo OT, Fawole B, Blum J, Abalos E. Advance distribution of misoprostol for preventing and treating excessive blood loss after birth. Cochrane Database of Systematic Reviews. February 15, 2012. ŌĆó National Population Commission (NPC) [Nigeria] and ICF. Nigeria Demographic and Health Survey 2018 Key Indicators Report. NPC and ICF; 2019. ŌĆó Meh C, Thind A, Ryan B, Terry A. Levels and determinants of maternal mortality in northern and southern Nigeria. BMC Pregnancy Childbirth. 2019; 19: 1- 13. ŌĆó Bohren MA, Lorencatto F, Coomarasamy A, et al. Formative research to design an implementation strategy for a postpartum haemorrhage initial response treatment bundle (E-MOTIVE): study protocol. Reprod Health. 2021; 18: 149. ŌĆó United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019: Data Booket. ST/ESA/SER. A/424. UN; 2019. ŌĆó Makinde OA, Sule A, Ayankogbe O, Boone D. Distribution of health facilities in Nigeria: implications and options for universal health coverage. Int J Health Plann Manage. 2018; 33: e1179- e1192.
- 28. ŌĆó Mutihir JT, Utoo BT. Postpartum maternal morbidity in Jos, North-Central Nigeria. Niger J Clin Pract. 2011; 14: 38- 42. ŌĆó Onyema OA, Cornelius AC, Uchenna ET, Duke OA. Primary postpartum haemorrhage in a Federal Medical Centre, Owerri, Nigeria: a six-year review. Niger J Med. 2015; 24: 242- 245. ŌĆó Galadanci H, K├╝nzel W, Zinser R, Shittu O, Adams S, Gruhl M. Experiences of 6 years quality assurance in obstetrics in Nigeria - a critical review of results and obstacles. J Perinat Med. 2016; 44: 301- 308. ŌĆó Muhammad R, Isah A, Agida T, Akaba G. A prospective study to compare the effectiveness of adjunctive rectal misoprostol or oxytocin titration in the prevention of primary post-partum haemorrhage in at-risk patients. Afr Health Sci. 2019; 19: 1517- 1524. ŌĆó DaŌĆÖu A, Kumurya AS, Bello MM, Galadanchi H, Getso KI. Availability of emergency obstetric care (EMOC) in Kano Metropolis, Nigeria. Int J Adv Case Rep. 2016; 3: 345- 353. ŌĆó Suarez S, Conde-Agudelo A, Borovac-Pinheiro A, et al. Uterine balloon tamponade for the treatment of postpartum haemorrhage: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020; 222: 293.e1- 293.e52.






















![ŌĆó Oladapo OT, Fawole B, Blum J, Abalos E. Advance distribution of misoprostol for
preventing and treating excessive blood loss after birth. Cochrane Database of
Systematic Reviews. February 15, 2012.
ŌĆó National Population Commission (NPC) [Nigeria] and ICF. Nigeria Demographic
and Health Survey 2018 Key Indicators Report. NPC and ICF; 2019.
ŌĆó Meh C, Thind A, Ryan B, Terry A. Levels and determinants of maternal mortality
in northern and southern Nigeria. BMC Pregnancy Childbirth. 2019; 19: 1- 13.
ŌĆó Bohren MA, Lorencatto F, Coomarasamy A, et al. Formative research to design
an implementation strategy for a postpartum haemorrhage initial response
treatment bundle (E-MOTIVE): study protocol. Reprod Health. 2021; 18: 149.
ŌĆó United Nations, Department of Economic and Social Affairs, Population Division.
World Population Prospects 2019: Data Booket. ST/ESA/SER. A/424. UN; 2019.
ŌĆó Makinde OA, Sule A, Ayankogbe O, Boone D. Distribution of health facilities in
Nigeria: implications and options for universal health coverage. Int J Health Plann
Manage. 2018; 33: e1179- e1192.](https://image.slidesharecdn.com/thescourgeofpphinnigeria-230814182310-2ac8ddbd/85/The-scourge-of-PPH-in-Nigeria-pptx-27-320.jpg)
















































