Tuberculosis management, pathophysiology and treatment.pptx
- 2. Introduction • Leading cause of infectious death • Disease caused by bacteria of Mycobacterium tuberculosis complex • Often affecting lung but can also involve other organs • Airbone spread by inhalation of inhalation of droplet nuclei produced by infectious individual with pulmonary TB
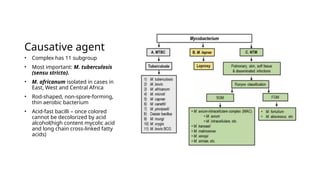
- 3. Causative agent • Complex has 11 subgroup • Most important: M. tuberculosis (sensu stricto). • M. africanum isolated in cases in East, West and Central Africa • Rod-shaped, non-spore-forming, thin aerobic bacterium • Acid-fast bacilli – once colored cannot be decolorized by acid alcohol(high content mycolic acid and long chain cross-linked fatty acids)
- 4. Epidemiology • In 2019, an estimated 10 million people developed TB and 1.5 million died from the disease. • 97% in low and middle income countries, Asia(6.4m), Africa (2.4m) • 8% associated with HIV co-infection of these 76% from Africa • More in males than females • In Kenya, upto 100,000 cases are reported annually.
- 5. Pathogenesis • Droplet nuclei aerosolized by coughing, sneezing or speaking • Remain in the air for several hours – reaching terminal airway when inhaled. • Exogenous factors for spread: • Probability of contact • Duration of contact • Intimacy of contact • Degree of infectiousness of the case • Smear positive contact • Cavitary pulmonary disease • HIV and TB co-infection: less infectious • Smear-negative/culture-positive vs culture-negative/extrapulmonary disease
- 6. • Exogenous factors for spread: • Degree of immune-competence: cancer pt on tx, HIV, pt on immunosuppressants • Risk of developing disease • Innate defense and cell-mediated immunity • Primary TB – disease occurring following infection: children/immuno-compromised • Secondary TB – infection occurs, bacilli are contained, reactivates later in life
- 7. • Infection begins when the droplet reach the alveoli • Myeloid dendritic cells are infected, macrophages phagocytose the bacilli. • The bacilli survive within the phagosome, replicates then ruptures releasing more bacilli that are ingested by other phagocytes. • Then bacilli disseminate widely in the lymphatic vessel to other parts of the lung or other organs attacking more macrophages. • The bacilli are presented to T lymphocytes in the draining lymph node where cell-mediated and humoral immunity
- 8. • Macrophage activating response – T cell response that leads to activation of macrophages that kill the mycobacteria • Macrophages present bacteria to T lymphocytes which in turn are activate to T-helper 1 (produce IFN gamma – activating more macrophages), T-helper 2: IL-4, 5, 10, 13) • Tissue damaging response – delayed type hypersensitivity leading to destruction of macrophages containing mycobacteria. • Granulomas are formed – named tubercles • Some lesions may heal by fibrosis • Latent TB infection(LTBI): balance that lead to infection containment
- 10. Clinical presentation • Pulmonary TB: • primary TB – fever and pleuritic chest pain, hilar lymphadenopathy, ghon focus vs ghon complex, middle and lower lobes • secondary – fever, night sweats, weigh loss, cough, purulent sputum with blood streaking, hemoptysis, localized in apical, posterior segment of upper lobes, superior segments of lower lobes.
- 11. • Extrapulmonary TB • Lymphadenitis – FNA, Excision for diagnosis • Pleural involvement – straw-colored fluid, exudative, ADA if low excludes TB • Genitourinary – dysuria, hematuria, flank pain, • Spine TB(Pott’s)- involving two or more adjacent bones • TB Meningitis – occur in HIV seropositive, over 1-2 weeks, cranial nerve palsy, CSF – lymphocytes, high protein and low glucose • Gastrointestinal – pain, hematochezia or mass – TB peritonitis • Pericarditis – fever, retrosternal dull pain, effusion, constrictive pericarditis • Miliary TB – hematogenous spread,
- 12. Post TB complications • Bronchiectasis • Aspergilloma • Chronic pulmonary aspergillosis
- 13. TB and HIV • TB causes 1/3 of HIV related deaths • Develops within weeks in HIV patients • Can be typical or atypical • Atypical: diffuse infiltrate, little or no cavitation, pleural effusion, more intrathoracic lymphadenopathy • Extrapulmonary TB is more common • TB immune reconstitution disease • Prevention: DO NOT INITIATE ART in the first 8 weeks of TB treatment, give prednisolone 1.5mg/kg for 2 weeks then half dose for 2 more weeks
- 14. Diagnosis • AFB microscopy(ZN, florescence microscpy) – examine 2 to 3 sputum samples • Cultures and DNA testing • Culture on liquid media – 2-3 weeks • Nucleic acid amplication – genexpert • Drug suscebility testing • TST vs IGRA – WHO recommends using of any to screen for TB esp. if initiating PTP
- 15. Treatment • Rifampicin: 600mg/day, cytochrome p450 inducer reduces bioavailabity of other drugs • Isoniazid 300mg/day – hepatotoxity and peripheral neuropathy(pyridoxine 50mg/day) • Ethambutol 15mg/kg/day – optic neuritis • Pyrizinamide 15-30mg/kg/day – hyperuricemia • Others • Streptomycin 750mg to 1 g/day • Rifabutin used in case of nnrti or pi • Rifapentin • Floroquinolones: levo, gati, moxifloxacin
- 16. monitoring • LFTs, symptoms of hepatitis • Stop all meds if ASTs are 5-6fold elevated • Reintroduce meds once LFTs normalizes one at a time
- 17. Kenya guidelines
Editor's Notes
- #3: the mycobacterial cell wall, lipids (e.g., mycolic acids) are linked to underlying arabinogalactan and peptidoglycan. This structure results in very low permeability of the cell wall, thus reducing the effectiveness of most antibiotics. Another molecule in the mycobacterial cell wall, lipoarabinomannan, is involved in the pathogen–host interaction and facilitates the survival of M. tuberculosis within macrophages.
- #15: All pulmonary TB re-treatment cases should have sputum TB culture and drug susceptibility testing to exclude drug resistance and especially multi-drug resistant TB. (2013, Kenya Guidelines)