UGI for MBBS 3 guide to history, examination and acute management
- 1. APPROACH TO UPPER GI BLEED Dr. Tim Mutafya Gen Surg. resident MBBS III class
- 2. OVERVIEW ŌĆó Definition & Epidemiology ŌĆó Classification ŌĆó Pathophysiology ŌĆó Clinical presentation ŌĆó Screening & Diagnosis ŌĆó Initial management
- 3. Definition Upper GIB is that originating proximal to the ligament of Treitz; ŌĆó from the oesophagus, stomach and duodenum
- 4. EPIDEMIOLOGY ŌĆó UGIB is more common than bleeding from the lower GI tract, accounting for 70% of all gastrointestinal bleeding. ŌĆó 80% are self-limited. ŌĆó Most common source is stomach and proximal duodenum due to peptic ulcer ŌĆó Pts on anti platelet therapy has two fold increase in bleed as compared to normal ones. ŌĆó 20% of pts of moderate to high risk, who have recurrent bleeding (within 48-72 hrs) have poor prognosis. ŌĆó The mortality rate is 5% to 10% for severe UGI bleed.
- 5. RISK FACTORS ŌĆó Age > 50 years, Male ŌĆó Drugs: Use of NSAIDS, antiplatelet ŌĆó H-pylori infection ŌĆó Excessive alcohol intake ŌĆó Excess acid production
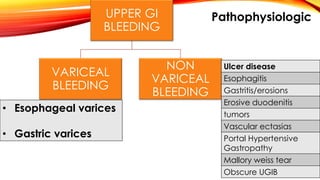
- 7. UPPER GI BLEEDING VARICEAL BLEEDING NON VARICEAL BLEEDING ŌĆó Esophageal varices ŌĆó Gastric varices Ulcer disease Esophagitis Gastritis/erosions Erosive duodenitis tumors Vascular ectasias Portal Hypertensive Gastropathy Mallory weiss tear Obscure UGIB Pathophysiologic
- 8. Anatomical
- 9. Major causes
- 10. Esophageal Varices Gastric ŌĆó Associated with high HPVG > 12mmHg ŌĆó About 40% of patients with cirrhosis and in 60% of patients with cirrhosis and ascites. ŌĆó Up to 25% of patients with newly diagnosed varices will bleed within two years. ŌĆó 80% will stop bleeding spontaneously. ŌĆó Can occur with HVPG less than 12 mm Hg ŌĆó High risk ŌĆó Not usually associated with cirrhosis o splenic vein thrombosis o Pancreatitis o pancreatic cancer.
- 11. Varices Prehepatic ŌĆó Portal venous thrombosis ŌĆó Infiltrative tumors Intrahepatic ŌĆó Schistosomiasis ŌĆó Liver cirrhosis ŌĆó Veno-occlusive disease Post hepatic ŌĆó Budd chiari syndrome
- 13. Most frequent cause of upper GI Bleeding Duodenal Ulcer-gastroduodenal A. PUD Gastric ulcer-left gastric A. PEPTIC ULCER DISEASE H.PYLORI: NSAIDS: * involves antrum * gastric ulcers > common *duodenal ulcers * 15-45% patients develop ulcers on regular use ŌĆó As the ulcer burrows deeper into the gastroduodenal mucosa,weakening and necrosis of the arterial wall,development of a pseudoaneurysm. ŌĆó weakened wall ruptures hemorrhage
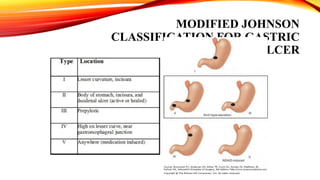
- 14. MODIFIED JOHNSON CLASSIFICATION FOR GASTRIC ULCER
- 15. Mallory weiss syndrome / tears ŌĆó Mucosal or sub-mucosal lacerations that occur at the gastro-esophageal junction and usually extend distally into a hiatal hernia . ŌĆó Typically have a history of recent non-bloody vomiting with excessive retching followed by hematemesis.. ŌĆó Endoscopy usually reveals a single tear that begins at the gastro-esophageal junction and extends several millimeters distally into a hiatal hernia sac/within cardiac portion of stomach.
- 16. Haemorragic/Erosive gastritis ŌĆó Stress related mucosal injury ŌĆó Occur mostly in extremly sick patients ŌĆó Major Trauma ŌĆó Post Major Surgery ŌĆó 3rd Degree burns ŌĆó Major intracranial disease ŌĆó Severe medical illness (Ventilator dependence, coagulopathy) ŌĆó Significant bleeding probably does not develop unless ulceration occurs. ŌĆó Intravenous H2-receptor antagonist is the treatment of choice. Sucralfate also effective ŌĆó Aspirin and NSAIDS ŌĆó Half of the patient who chronically ingest NSAIDS have Erosions. (15 ŌĆō 30% have Ulcers) ŌĆó Most Frequently and severely affected site is gastric antrum.
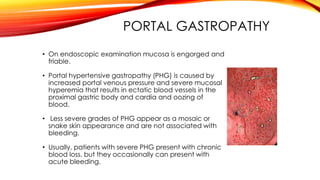
- 17. PORTAL GASTROPATHY ŌĆó On endoscopic examination mucosa is engorged and friable. ŌĆó Portal hypertensive gastropathy (PHG) is caused by increased portal venous pressure and severe mucosal hyperemia that results in ectatic blood vessels in the proximal gastric body and cardia and oozing of blood. ŌĆó Less severe grades of PHG appear as a mosaic or snake skin appearance and are not associated with bleeding. ŌĆó Usually, patients with severe PHG present with chronic blood loss, but they occasionally can present with acute bleeding.
- 18. DIEULAFOY'S LESION ŌĆó It is a large (1- to 3-mm) submucosal artery that protrudes through the mucosa. ŌĆó It is not associated with a peptic ulcer, and can cause massive bleeding. ŌĆó It usually is located in the gastric fundus, within 6 cm of the gastroesophageal junction. ŌĆó Dieulafoy's lesion can be difficult to identify at endoscopy because of the intermittent nature of the bleeding. ŌĆó the overlying mucosa may appear normal if the lesion is not bleeding.
- 19. GASTRIC ANTRAL VASCULAR ECTASIA ŌĆó Gastric antral vascular ectasia (GAVE), also described as watermelon stomach. ŌĆó Characterized by rows or stripes of ectatic mucosal blood vessels that emanate from the pylorus and extend proximally into the antrum . ŌĆó Unknown etiology ŌĆó Common in older women and patients with ESRD
- 20. Aortoenteric fistula ŌĆó The A-E fistula is a communication between the native abdominal aorta and, most commonly, the third portion of the duodenum. ŌĆó Bleeding is usually acute and massive, with a high mortality rate(30-100%). ŌĆó Often, a self-limited herald bleed occurs hours to months before a more severe, exsanguinating bleed. ŌĆó The fistula usually forms between three and five years after graft placement.
- 21. Presentation
- 22. 1. Hematemesis ŌĆó Vomiting of red blood or coffee- grounds material when gastric acid converts hemoglobin into methemoglobin . Differentiate from :- ’āśHemoptysis. ’āśBleeding from Pharynx , nasal passage USUALLY hematemesis requires a bucket; BUT haemoptysis a small bowl.
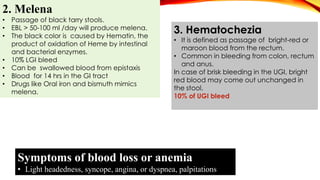
- 23. 2. Melena ŌĆó Passage of black tarry stools. ŌĆó EBL > 50-100 ml /day will produce melena. ŌĆó The black color is caused by Hematin, the product of oxidation of Heme by intestinal and bacterial enzymes. ŌĆó 10% LGI bleed ŌĆó Can be swallowed blood from epistaxis ŌĆó Blood for 14 hrs in the GI tract ŌĆó Drugs like Oral iron and bismuth mimics melena. 3. Hematochezia ŌĆó It is defined as passage of bright-red or maroon blood from the rectum. ŌĆó Common in bleeding from colon, rectum and anus. In case of brisk bleeding in the UGI, bright red blood may come out unchanged in the stool. 10% of UGI bleed Symptoms of blood loss or anemia ŌĆó Light headedness, syncope, angina, or dyspnea, palpitations
- 24. Aetiology Leading history MalloryWeiss tear Multiple Emesis before hematemesis, alcoholism, retching Esophageal ulcer Dysphagia, Odynophagia, GERD Peptic ulcer Epigastric pain, NSAID or aspirin use Stress gastritis Patient in an ICU, gastrointestinal bleeding occurring after admission,respiratory failure,multiorgan failure,coagulopathy Varices, portal gastropathy Alcoholism, Cirrhosis of liver Gastric antral vascular ectasia Renal failure, cirrhosis Malignancy Recent involuntary weight loss, dysphagia, cachexia, early satiety Angiodysplasia Chronic renal failure, hereditary hemorrhagic telangiectasia Aortoenteric fistula Known aortic aneurysm, prior abdominal aortic aneurysm repair Clues regarding the cause of acute UGI bleeding
- 25. ŌĆó Pallor , signs of dehydration , Shock ŌĆó Icterus ŌĆó Clubbing ŌĆó Oedema }Liver disease Physical Examination
- 26. Lymphadenopathy VirchowŌĆÖs Node (TroisierŌĆÖs sign) Vital signs Tachycardia Hypotension Tachypnea
- 27. ŌĆó Ascites ŌĆó Spider naevi ŌĆó Palmar erythema ŌĆó DupuytrenŌĆÖs contracture
- 28. ŌĆó Leuconychia ŌĆó Gynecomastia ŌĆó Bleeding manifestations ŌĆó Scars of previous surgery
- 29. ŌĆó Splenomegaly ŌĆó Caput medusae ŌĆó Parotid Swelling ŌĆó Fetor hepaticus ŌĆó Asterixis ŌĆó Testicular atrophy ŌĆó Acanthosis nigricans ŌĆó Alopecia ŌĆó Glossitis ŌĆó Loss of Axillary hair ŌĆó Loss of Pubic Hair
- 30. Inspection Distention , Dilated Veins Swelling Visible peristalsis Palpation Tenderness HSM, secondary metastasis Sister Mary Joseph nodules Mass Percussion Shifting dullness HSM Auscultation Absent Bowel sound Bruit Cruveilhier-Baumgarten venous hum ABDOMEN EXAMINATION
- 31. APPROACH TO A PATIENT WITH UGIB Immediate Initial Assessment Stabilization of haemodynamic status Identify bleed source Stop active bleed Treat underlying cause Prevent recurrence of bleeding
- 32. Risk assessment & triage Risk for mortality and rebleeding. Categorised as ’ā¼ low, ’ā¼ intermediate ’ā¼ high risk Record the GCS Poo prognostic factors 1. Age over 60 2. Shock(SBP<100mmhg), pulse >100 3. Malignancy or varices as bleeding source. 4. Severe coagulopathy 5. Comorbid medical illness 6. Continued or recurrent bleeding 7. Multi-organ failure
- 33. Workup Bloods ŌĆó Hematology - FBC, G+ crossmatch ŌĆó Biochemistry- U&Es, LFT+ albumin ŌĆó Serology - H-pylori, Hep B/C,HIV, schistosomiasis ŌĆó Coagulation profile ŌĆó Stool: occult blood Imaging ŌĆó Esophagogastroduodenoscopy o Therapeutic and diagnostic ŌĆó CXR ŌĆó ECG ŌĆó Abdominal USS ŌĆó CT Angiography
- 34. MANAGEMENT OF UGIB GENERAL MEDICAL MANAGEMENT TYPE OF BLEEDING VARICEAL BLEEDING NON VARICEAL BLEEDING MEDICAL ENDOTHERAPY SURGICAL INERVENTION PRESSURE TECHNIQUES
- 35. AUGIB Rapid Assessment Monitor Hemodynamic Status Fluid Resuscitation Ryle;s tube for Gastric Lavage Self Limited Hemorrhage (80%) Continued bleeding (10-25%) Urgent endoscopy Recurrent Hemorrhage Elective Endoscopy (With in 24 ŌĆō 48 hours) Definitive Therapy (If Necessary) Site not localized Localized Further Assessment (Extended EGD, Radio-isotope scan, Arteriography, Exploratory Definitive