Update management of CAP
- 2. BY Dr. Assuit University Lecturer of Chest Diseases
- 4. âĒ Richard G. Wunderink and Grant W. Waterer. Community-Acquired Pneumonia. N Engl J Med 2014;370:543-51. DOI: 10.1056/NEJMcp1214869 âĒ Infectious Diseases Society of America (IDSA) /American Thoracic Society Consensus (ATS) Guidelines on the Management of Community- Acquired Pneumonia in Adults. Clinical Infectious Diseases 2007; 44:S27â72.
- 5. The antibiotic regimens advocated by a collaboration between the Infectious Diseases Society of America (IDSA)/American Thoracic Society (ATS) in 2007 and the British Thoracic Society (BTS) in 2009.
- 7. Community-acquired pneumonia (CAP) is one of the most common infectious diseases and is an important cause of mortality and morbidity worldwide.
- 8. ïķ3.5 million cases/year ïķAt least 1 million hospitalizations/year ïķ9th leading cause of infectious death in US ïķ30 day morality for hospitalized patients is up to 23% ïķ$17 billion/year in healthcare costs in US
- 11. Pneumonia is acute infection of the lung parenchyma. Community-acquired pneumonia (CAP): Refers to pneumonia acquired outside of hospitals in the community and not acquired in a hospital, long-term care facility, or other recent contact with the health care system.
- 13. Typical community-acquired pneumonia The term âtypicalâ CAP refers to a bacterial pneumonia caused by pathogens such as S pneumoniae, H influenzae, and M catarrhalis. Patients with typical CAP classically present with fever, a productive cough with purulent sputum, dyspnea, and pleuritic chest pain.
- 14. Characteristic pulmonary findings on physical examination include the following: ïķ Tachypnea ïķ Rales heard over the involved lobe or segment ïķ Increased tactile fremitus, bronchial breath sounds, and egophony may be present if consolidation has occurred. ïķ Decreased tactile fremitus and dullness on chest percussion may result from parapneumonic effusion or empyema.
- 15. Atypical community-acquired pneumonia The clinical presentation of so-called âatypicalâ CAP is often subacute and frequently indolent. In addition, patients with atypical CAP may present with more subtle pulmonary findings, nonlobar infiltrates on radiography, and various extrapulmonary manifestations (eg, diarrhea, otalgia).
- 16. Atypical CAP pathogens include the following: ïķ Mycoplasma pneumoniae ïķ Chlamydophila ( Chlamydia) pneumoniae ïķ Legionnaires disease (Legionella pneumophila) ïķ Respiratory viruses :Influenza A and B, Rhinovirus and Respiratory syncytial virus.
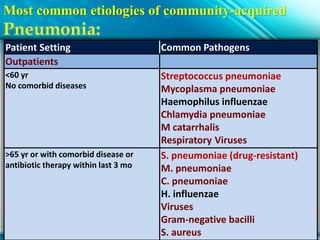
- 17. Most common etiologies of community-acquired Patient Setting Common Pathogens Outpatients <60 yr No comorbid diseases Streptococcus pneumoniae Mycoplasma pneumoniae Haemophilus influenzae Chlamydia pneumoniae M catarrhalis Respiratory Viruses >65 yr or with comorbid disease or antibiotic therapy within last 3 mo S. pneumoniae (drug-resistant) M. pneumoniae C. pneumoniae H. influenzae Viruses Gram-negative bacilli S. aureus
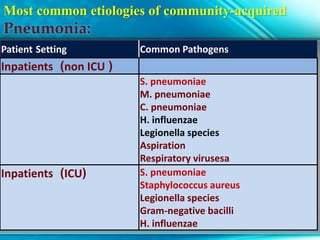
- 18. Most common etiologies of community-acquired Patient Setting Common Pathogens (non ICU)Inpatients S. pneumoniae M. pneumoniae C. pneumoniae H. influenzae Legionella species Aspiration Respiratory virusesa (ICU)Inpatients S. pneumoniae Staphylococcus aureus Legionella species Gram-negative bacilli H. influenzae
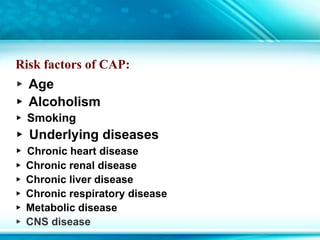
- 20. Risk factors of CAP: âļ Age âļ Alcoholism âļ Smoking âļ Underlying diseases âļ Chronic heart disease âļ Chronic renal disease âļ Chronic liver disease âļ Chronic respiratory disease âļ Metabolic disease âļ CNS disease
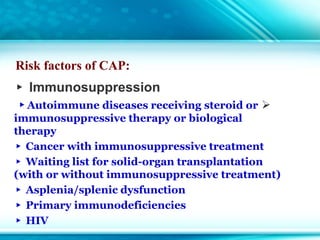
- 21. Risk factors of CAP: âļ Immunosuppression ïâļAutoimmune diseases receiving steroid or immunosuppressive therapy or biological therapy âļ Cancer with immunosuppressive treatment âļ Waiting list for solid-organ transplantation (with or without immunosuppressive treatment) âļ Asplenia/splenic dysfunction âļ Primary immunodeficiencies âļ HIV
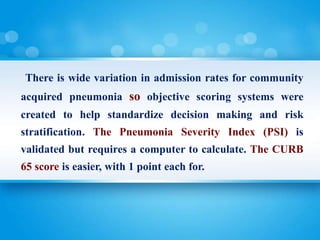
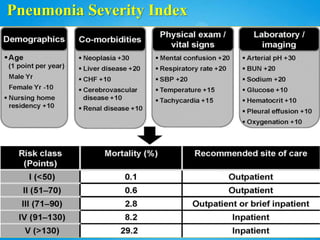
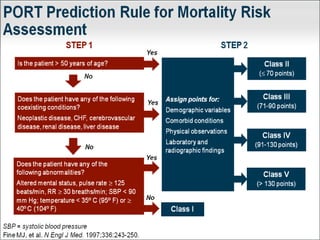
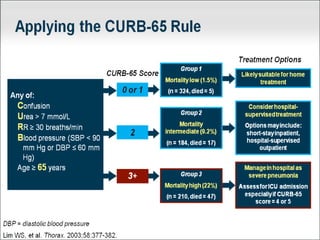
- 22. There is wide variation in admission rates for community acquired pneumonia so objective scoring systems were created to help standardize decision making and risk stratification. The Pneumonia Severity Index (PSI) is validated but requires a computer to calculate. The CURB 65 score is easier, with 1 point each for.
- 26. severe community-acquired pneumonia: Several criteria have been proposed to define severe CAP. Most case series have defined it simply as CAP that necessitates ICU admission
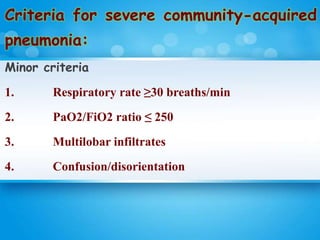
- 27. Criteria for severe community-acquired pneumonia: Minor criteria 1. Respiratory rate âĨ30 breaths/min 2. PaO2/FiO2 ratio âĪ 250 3. Multilobar infiltrates 4. Confusion/disorientation
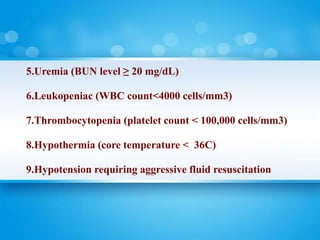
- 28. 5.Uremia (BUN level âĨ 20 mg/dL) 6.Leukopeniac (WBC count<4000 cells/mm3) 7.Thrombocytopenia (platelet count < 100,000 cells/mm3) 8.Hypothermia (core temperature < 36C) 9.Hypotension requiring aggressive fluid resuscitation
- 29. Major criteria âĒ Invasive mechanical ventilation âĒ Septic shock with the need for vasopressors
- 30. Diagnosing Pneumonia: How Much Testing Is Needed?
- 31. No diagnostic testing beyond chest radiograph is necessary for most people with community acquired pneumonia, especially outpatients or those hospitalized with less severe disease. Among people with more severe pneumonia, there is disagreement among experts as to how much diagnostic testing is indicated
- 32. Purulent sputum is characteristic of pneumonia caused by bacterial community-acquired pneumonia (CAP) pathogens and is not usually a feature of pneumonia caused by atypical pathogens. Blood-tinged sputum may be found in patients with pneumococcal pneumonia, Klebsiella pneumonia, or Legionella pneumonia. Rales are heard over the involved lobe or segment. Consolidation may be accompanied by an increase in tactile fremitus, bronchial breathing, and egophony.
- 33. Investigations Blood culture: These authors recommend blood culture only for patients admitted to the ICU or with healthcare associated pneumonia, or who have cirrhosis or lack a spleen. Sputum culture: For intubated patients, or those with productive cough with severe pneumonia or HCAP or severe COPD or structural lung disease (e.g. bronchiectasis).
- 34. During influenza season, testing for influenza is indicated for all patients with pneumonia, with treatment with oseltamivir if flu testing is positive (or empirically pending influenza test results). Urinary pneumococcal and Legionella antigen testing is recommended for people with severe or health care associated pneumonia. Pleural fluid should be always cultured, if it is collected
- 35. Treatment
- 36. The primary concern when selecting antibiotics for community acquired pneumonia is ensuring coverage of Streptococcus pneumoniae and atypical organisms including Mycoplasma, Chlamydophila, and Legionella. Treatment should always be individualized, but published recommendations by the IDSA and ATS have suggested the following:
- 37. Empirical Antimicrobial Therapy for CAP Patient Setting Empirical Therapy Outpatients Previously healthy and no use of antimicrobials within the previous 3 months o Macrolide (strong recommendation; level I evidence) o Doxycyline (weak recommendation; level III evidence)ycycline Presence of comorbidities such as chronic heart, lung, liver or renal disease; diabetes mellitus; alcoholism; malignancies; asplenia; immunosuppressing conditions. o A respiratory fluoroquinolone (moxifloxacin, gemifloxacin, or levofloxacin [750 mg]) (strong recommendation; level I evidence) o A b-lactam plus a macrolide (strong recommendation; level Ievidence)
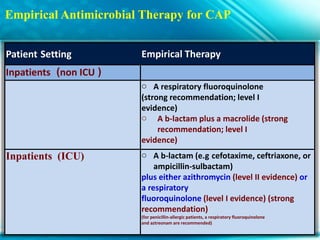
- 38. Empirical Antimicrobial Therapy for CAP Patient Setting Empirical Therapy (non ICU)Inpatients o A respiratory fluoroquinolone (strong recommendation; level I evidence) o A b-lactam plus a macrolide (strong recommendation; level I evidence) (ICU)Inpatients o A b-lactam (e.g cefotaxime, ceftriaxone, or ampicillin-sulbactam) plus either azithromycin (level II evidence) or a respiratory fluoroquinolone (level I evidence) (strong recommendation) (for penicillin-allergic patients, a respiratory fluoroquinolone and aztreonam are recommended)
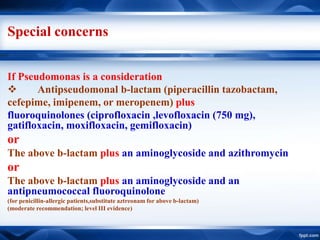
- 39. Special concerns If Pseudomonas is a consideration ïķ Antipseudomonal b-lactam (piperacillin tazobactam, cefepime, imipenem, or meropenem) plus fluoroquinolones (ciprofloxacin ,levofloxacin (750 mg), gatifloxacin, moxifloxacin, gemifloxacin) or The above b-lactam plus an aminoglycoside and azithromycin or The above b-lactam plus an aminoglycoside and an antipneumococcal fluoroquinolone (for penicillin-allergic patients,substitute aztreonam for above b-lactam) (moderate recommendation; level III evidence)
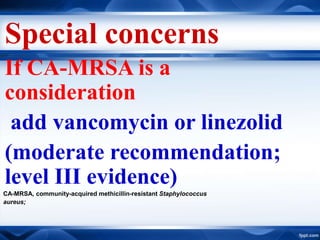
- 40. Special concerns If CA-MRSA is a consideration add vancomycin or linezolid (moderate recommendation; level III evidence) CA-MRSA, community-acquired methicillin-resistant Staphylococcus aureus;
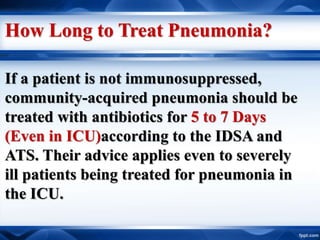
- 41. How Long to Treat Pneumonia? If a patient is not immunosuppressed, community-acquired pneumonia should be treated with antibiotics for 5 to 7 Days (Even in ICU)according to the IDSA and ATS. Their advice applies even to severely ill patients being treated for pneumonia in the ICU.
- 42. Who Should Get Broad- Spectrum Antibiotics for Pneumonia?
- 43. Those patients with pneumonia and certain risk factors : 1. hospitalized or receiving antibiotics within 90 days, 2. nursing home residence, hemodialysis, home wound care, 3. immunosuppression, 4. a family member with a multidrug resistant organism, poor functional status
- 44. Those patients are more likely to have pneumonia due to drug-resistant bacteria. They may fail standard therapy for community acquired pneumonia, and have been termed as having healthcare associated pneumonia (HCAP).
- 45. Until recently, many experts have advised that ïķ Most such HCAP patients be treated with two anti- Pseudomonas agents and coverage for MRSA. However the concept of HCAP, and the implication that all such patients should initially be treated with broad spectrum antibiotics, are considered controversial today, because the scheme leads to overuse of broad agents. ïķ The risk justifies MRSA coverage, but not dual coverage for Pseudomonas
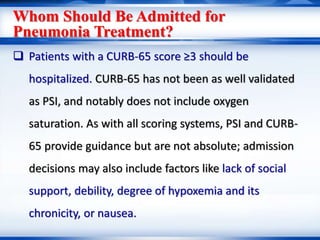
- 46. Whom Should Be Admitted for Pneumonia Treatment? ïą Patients with a CURB-65 score âĨ3 should be hospitalized. CURB-65 has not been as well validated as PSI, and notably does not include oxygen saturation. As with all scoring systems, PSI and CURB- 65 provide guidance but are not absolute; admission decisions may also include factors like lack of social support, debility, degree of hypoxemia and its chronicity, or nausea.
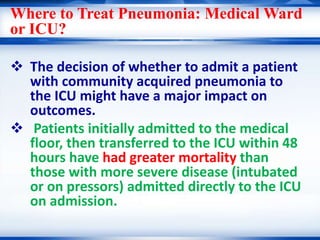
- 47. Where to Treat Pneumonia: Medical Ward or ICU? ïķ The decision of whether to admit a patient with community acquired pneumonia to the ICU might have a major impact on outcomes. ïķ Patients initially admitted to the medical floor, then transferred to the ICU within 48 hours have had greater mortality than those with more severe disease (intubated or on pressors) admitted directly to the ICU on admission.
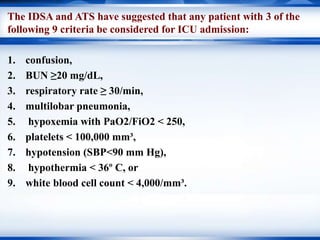
- 48. The IDSA and ATS have suggested that any patient with 3 of the following 9 criteria be considered for ICU admission: 1. confusion, 2. BUN âĨ20 mg/dL, 3. respiratory rate âĨ 30/min, 4. multilobar pneumonia, 5. hypoxemia with PaO2/FiO2 < 250, 6. platelets < 100,000 mmÂģ, 7. hypotension (SBP<90 mm Hg), 8. hypothermia < 36š C, or 9. white blood cell count < 4,000/mmÂģ.
- 49. The use of systemic corticosteroids in patients with CAP? ïķ May reduce the length of time until clinical stability, reduce hospital length of stay, reduce the need for mechanical ventilation, and reduce the incidence of adult respiratory distress syndrome (ARDS). ïķ Recent clinical trials have also shown a possible overall reduction in mortality, although these later results remain in doubt.
- 50. The use of systemic corticosteroids in patients with CAP? ïķ However ,there is insufficient data or agreement on the dose or duration of the steroid therapy. ïķ There are current ongoing double-blind, randomized, controlled clinical trials to examine the short- and long-term effects of corticosteroid use in the management of CAP.
- 51. The use of systemic corticosteroids in patients with CAP ïķ may reduce the length of time until clinical stability, reduce hospital length of stay, reduce the need for mechanical ventilation, and reduce the incidence of adult respiratory distress syndrome (ARDS). [49, 50] Recent clinical trials have also shown a possible overall reduction in mortality, although these later results remain in doubt. [51, 52] Furthermore,
Editor's Notes
- PSI has been around the longest & been validated more widely butâĶ cumbersome!
- ERS/ATS GUIDELINES ON SEVERE ASTHMA | K.F. CHUNG ET AL





![Empirical Antimicrobial Therapy for CAP
Patient Setting Empirical Therapy
Outpatients
Previously healthy and no use of
antimicrobials within the
previous 3 months
o Macrolide (strong
recommendation; level I evidence)
o Doxycyline (weak
recommendation; level III
evidence)ycycline
Presence of comorbidities such as
chronic heart, lung, liver
or renal disease; diabetes mellitus;
alcoholism; malignancies;
asplenia; immunosuppressing
conditions.
o A respiratory fluoroquinolone
(moxifloxacin, gemifloxacin, or
levofloxacin [750 mg]) (strong
recommendation; level I
evidence)
o A b-lactam plus a macrolide
(strong recommendation; level
Ievidence)](https://image.slidesharecdn.com/cap-180312080631/85/Update-management-of-CAP-37-320.jpg)
![The use of systemic corticosteroids in
patients with CAP
ïķ may reduce the length of time until
clinical stability, reduce hospital length
of stay, reduce the need for mechanical
ventilation, and reduce the incidence of
adult respiratory distress syndrome
(ARDS). [49, 50] Recent clinical trials
have also shown a possible overall
reduction in mortality, although these
later results remain in doubt. [51, 52]
Furthermore,](https://image.slidesharecdn.com/cap-180312080631/85/Update-management-of-CAP-51-320.jpg)
