vascular supply of brain and spinal cord - Copy.pptx
- 1. Vascular supply 0f brain(applied) Presenter: DR. F. M. Monjur Hasan FCPS Neurology trainee
- 2. Introduction ’ü▒Among all the neurologic diseases of adult life cerebrovascular disease ranks first in frequency and importance. ’ü▒Occlusion of cerebral blood vessels is the commonest. ’ü▒Knowledge of the stroke syndromes, the signs and symptoms that correspond to the region of brain that is supplied by each vessel, allows a degree of precision in determining the particular vessel that is occluded . ’ü▒The anatomical diversity of cerebral vasculature leads to different clinical presentation and outcome of a given arterial occlusion among different individual
- 3. Collateral status Collaterals are direct anastomoses between cerebral blood vessels that allow rerouting of blood flow when direct blood supply is blocked to brain tissue
- 4. Stroke syndrome ’ü▒The identification of the stroke syndromes by careful clinical examination is one of the cardinal skills of the clinical neurologist. ’ü▒Stroke syndrome is particularly applied for ischemia and infarct. ’ü▒In hemorrhage the total clinical picture may be different. ’ü▒Not all vascular supply is clinically common and important, hence today we will focus most practical and important aspects of cerebral circulation that we have to face in our daily patient encounter.
- 5. Stroke syndromes Anterior cerebral artery stroke syndromes Middle cerebral artery stroke syndromes Posterior cerebral artery stroke syndrome Basilar artery stroke syndrome
- 6. Stroke syndromes Superior cerebellar artery syndrome AICA syndrome PICA syndrome Vertebral artery stroke syndrome
- 7. Stroke syndrome Internal carotid artery syndrome Anterior choroidal artery syndrome Subclavian artery syndrome Innominate artery syndrome
- 8. Anterior cerebral artery syndrome Cortical branch Anterior 3/4th of medial surface of frontal lobe Anterior 4/5th of Corpus callosum Deep branch Anterior limb of IC head of caudate globus pallidus
- 9. Paracentral lobule Function: motor & sensory area for foot, leg & UB Supply: pericallosal branch of ACA
- 10. ACA occlusion distal to Acom ’ü▒Contralateral sensorimotor deficit foot & leg sparing the face and arm ’ü▒Head and eyes may deviate towards the sight of lesion ’ü▒Urinary incontinence ’ü▒Gagenhalten of the opposite limb ’ü▒Sympathetic apraxia of left hand & alien limb phenomena
- 11. A1 occlusion if single ACA stem ’ü▒Paraplegia ’ü▒Abulia ’ü▒Memory impairment ’ü▒Incontinence ’ü▒Gagenhalten
- 12. Occlusion of recurrent artery of HeubnerŌĆÖs (RAH) Caudate Anterior limb Internal capsule Dysarthria and abulia Contralateral weakness of face & arm without sensory loss Agitation and hyperactivity choreoathetosis
- 13. Watershed or boarder zone infarct carotid stenosis plus circulatory collapse
- 14. Man in barrel syndrome in ACA-MCA border zone infarct
- 15. BalintŌĆÖs syndrome Asimultagnosia Optic ataxia Oculomotor apraxia Bilateral MCA-PCA boarder zone infarct
- 16. Limb shaking TIA Cerebral hypoperfusion of the ACA-MCA water shade zone Face is usually not involved Revascularization highly effective
- 17. Superficial cortical MCA territory
- 18. Internal capsule Fiber Vascular supply Deficit Anterior limb Frontopontine fiber Artery of Heubner Contralateral hemiplegia Genu Corticonuclear & corticobulbar to facial and hypoglossal Anterior choroidal, MCA Faciolingual syndrome Posterior limb Corticospinal Corticonuclear Corticobulbar MCA, anterior choroidal Contralateral hemiplegia
- 19. MCA territory Superficial cortical branch ŌĆó Motor area ŌĆó BrocaŌĆÖs area ŌĆó Sensory cortex ŌĆó Angular and supramarginal gyri ŌĆó Superior temporal gyrus & insula ŌĆó Wernicke area Deep penetrating branch ŌĆó Putamen ŌĆó Caudate head and body(shared with Heubner artery) ŌĆó Outer globus pallidus ŌĆó Posterior limb of internal capsule & corona radiata
- 20. MCA occlusion Main stem(M1) occlusion both proximal and distal Upper cortical Lower cortical Lentriculostriate
- 21. MCA main stem M1 occlusion Contralateral hemiplegia Leg and foot partly spared Contralateral hemi anaesthesia Deviation of head and eye towards the lesion Global aphasia
- 22. Lacunar stroke (lacune: 3-15 mm) ŌĆó Small arteries : 50-200 micrometer ŌĆó Enlarged Virchow -Robin space ŌĆó Absent of cortical deficit ŌĆó Mechanism: lipohyalinosis, trunk vessel atherosclerosis, embolic
- 23. Atypical vascular syndrome Putaminal vascular lesion can cause dystonic captocromia Caudate head stroke(MCA): starfish hand
- 24. Superior division MCA occlusion ( Rolandic and pre-Rolandic area) Discriminative features ŌĆó Effortful, hesitant, grammatically simplified or severe aphasia to the point of mutism ŌĆó No impairment of alertness ŌĆó No field defect
- 25. Distal branch of superior division occlusion Most common Ascending frontal branch occlusion: motor deficit limited to face & arm Left sided lesion: dysfluent agrammatic speech Left Rolandic branch occlusion: Sensorimotor paresis with severe dysarthria but little aphasia. Cortical-subcortical branch occlusion: Brachial monoplegia or hand weakness Anterior parietal branch occlusion: Only conduction aphasia & ideomotor apraxia, no sensorimotor deficit
- 27. Inferior division MCA occlusion ’ü▒ Lateral temporal ’ü▒ Inferior parietal lobe ’ā╝ Prominent receptive language deficit ’ā╝ Superior quadrantanopia ’ā╝ Gerstman syndrome ’ā╝ Alexia with agraphia
- 28. Gerstmann syndrome Site of lesion: Angular & supramarginal gyri Dominant Inferior parietal lobe, area 39 Artery block: inferior superficial MCA
- 29. Posterior circulation stroke syndrome
- 30. PCA syndrome
- 31. Blood supply of Thalamus ’ü▒Arteriolar vascular territory cross the nuclear boundary ’ü▒Timing has particular impact on clinical expression
- 32. PCA occlusion Proximal PCA syndrome Cortical ŌĆó Medial occipital ŌĆó Inferior temporal Bilateral
- 33. Atherosclerosis and dissection is common in vertebral and BA but not common in PCA where occlusion is mostly embolic ’ü▒ Atherothrombotic ’ü▒ Embolic ’ü▒ Dissection ’ü▒ Dolichoectasia
- 34. Artery occlusion Structure involved Deficit Interpeduncular branch AOP central midbrain and thalamus Vertical gaze palsy and coma Thalamoperforate branches Anteromedial inferior thalamic syndrome Hemiballism(Luys) , hemichorea Deep sensory loss, hemiataxia, tremor Thalamogeniculate Geniculate body thalamus Dejerine Roussy syndrome Paramedian vessels 3rd CN Red nucleus WeberŌĆÖs syndrome BenedictŌĆÖs syndrome Claude syndrome Bilateral PCA Bilateral occipital cortex Cortical blindness
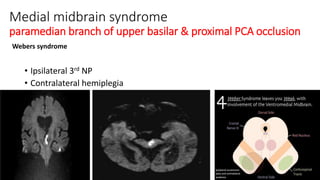
- 35. Medial midbrain syndrome paramedian branch of upper basilar & proximal PCA occlusion Webers syndrome ŌĆó Ipsilateral 3rd NP ŌĆó Contralateral hemiplegia
- 36. Ipsilateral 3rd nerve palsy Contralateral ataxia, tremor Contralateral choreoathetoid movement Small penetrating artery from PCA
- 37. ClaudeŌĆÖs syndrome Mid brain tegmental lesion Ipsilateral 3rd nerve palsy Contralateral ataxia and tremor No chorea or athetosis
- 38. Cortical syndrome of PCA (occipital) Contralateral incomplete homonymus hemianopia with macular sparing Visual hallucination in the blind part Metamorphopsia or Palinopsia
- 39. left PCA occlusion ŌĆó Alexia without agraphia ŌĆó Colour anomia ŌĆó Unable to name object and photograph
- 40. Bilateral PCA stroke syndrome Cortical blindness BalintŌĆÖs syndrome Prosopagnosia
- 41. Eyes Are Useless When the Mind Is Blind: Anton-Babinski Syndrome Obvious evidence of Cortical blindness Denial of blindness Confabulation
- 42. Prosopagnoasia PCA occlusion ’ü▒ Can see and describe face but unable to identify ’ü▒ Occipito-temporal association cortex ’ü▒ Fusiform gyrus
- 43. Vascular thalamic syndrome Paramedian thalamic infarct ŌĆó Apathy ŌĆó Somnolent ŌĆó Memory loss ŌĆó Vertical gaze abnormality ŌĆó Sleep and body core temperature abnormality ŌĆó Eyelid tremor Thalamogeniculate infarct Pure sensory or sensoriomotor stroke Thalamic syndrome of Dejerine Roussy
- 44. AOP infarct T2 & FLAIR DWI & ADC
- 45. Anterior thalamic syndrome Fluctuating level of consciousness Facial paresis of emotional movement Apathy & verbal perseveration Semantic memory loss Frontal lobe deficit Language deficit Posterior thalamic Quadrantanopia or sectoranopia Asymmetry of optokinetic nystagmus Hemi hypesthesia Thalamic aphasia
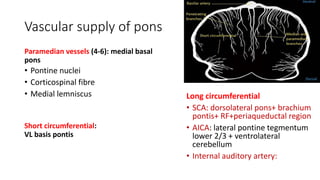
- 47. Vascular supply of pons Paramedian vessels (4-6): medial basal pons ŌĆó Pontine nuclei ŌĆó Corticospinal fibre ŌĆó Medial lemniscus Long circumferential ŌĆó SCA: dorsolateral pons+ brachium pontis+ RF+periaqueductal region ŌĆó AICA: lateral pontine tegmentum lower 2/3 + ventrolateral cerebellum ŌĆó Internal auditory artery: Short circumferential: VL basis pontis
- 48. Mid pontine paramedian base is most vulnerable during pontine ischemia in BA occlusion ŌĆó Arteries for Pontine tegmentum arise from distal basilar when these are patent tegmentum is relatively spared ŌĆó PICA & AICA, PICA &SCA anastomoses located in the lateral aspect of pons supplying the lateral tegmentum and basal structure of pons ŌĆó Largest penetrating artery supplying paramedian pons arise directly from BA
- 49. Basilar artery occlusion Asymmetry but bilaterality is the rule Herald hemiparesis may be present Motor or reflex abnormality in non hemiparetic site Slowly progressive & fluctuating
- 50. Motor, oculomotor and altered LOC presentation of BA occlusion Paramedian pontine base ŌĆó Long descending motor tract ŌĆó Crossing cerebellar fiber Paramedian pontine tegmentum ŌĆó Oculomotor fiber
- 51. Basilar Top syndrome (Embolic) ŌĆó Visual and oculomotor deficit ŌĆó Somnolent & death like behavior ŌĆó Sudden death or LOC
- 52. Pontine syndrome ŌĆó Ventral pontine syndrome ŌĆó Dorsal pontine syndrome ŌĆó Paramedian pontine syndrome ŌĆó Lateral pontine syndrome
- 53. Ventral pontine syndrome ŌĆó Millard-Gubler syndrome: VI & VII nerve fascicle+ contralateral hemiplegia ŌĆó Raymond syndrome: VI+ contralateral hemiplegia ŌĆó Pure motor hemiparesis: basis pontis ŌĆó Dysarthria-clumsy hand syndrome:basis pontis junction Upper 1/3 & lower 2/3rd ŌĆó Ataxic hemiparesis ŌĆó Locked-in syndrome: bilateral ventral pontine lesion
- 54. Locked-in syndrome complete pontine and lower midbrain infarction
- 55. Dorsal pontine syndrome Foville syndrome: ’ü▒ipsilateral 7th + contralateral hemiplegia+gaze away from lesion ’ü▒caudal tegmental Raymond-cestan syndrome Cerebellar ataxia with rubral tremor + contralateral sensory loss Rostral
- 56. Pontine syndrome ’ü▒Lateral superior pontine syndrome (SCA) ’ü▒Lateral mid pontine syndrome (short circumferential artery) ’ü▒Lateral inferior pontine syndrome (AICA) ’ü▒Medial superior pontine syndrome paramedian branch of upper basilar ’ü▒Medial mid pontine syndrome paramedian branch of mid basilar artery ’ü▒Medial inferior pontine syndrome paramedian branch of basilar artery
- 57. Blood supply of cerebellum SCA Superior surface of cerebellar hemisphere Superior vermis, dentate nucleus Upper MCP SCP Lateral pontine tegmentum AICA Anterior inferior cerebellum Flocculous Lower MCP Lateral pontomedullary tegmentum PICA Posterior inferior half of cerebellum Inferior vermis ICP Dorsolateral medulla
- 58. Superior cerebellar artery occlusion (dorsal cerebellar syndrome), superior half of cerebellar hemisphere, superior vermis, SCP, part of upper lateral pons ’ü▒ Ipsilateral cerebellar limb ataxia(MCP, SCP) ’ü▒ Nausea, vomiting & slurring of speech ’ü▒ Contralateral spinothalamic sensory loss ’ü▒ Partial deafness, ipsilateral HornerŌĆÖs syndrome ’ü▒ Ataxic tremor of ipsilateral upper extremity ’ü▒ Only dysarthria and unsteady gait may selectively occur due to peripheral branch occlusion
- 59. AICA occlusion lateral inferior pontine syndrome AICA supply inferolateral pons, inner ear, MCP and anterior inferior cerebellum Unilateral deafness & facial paralysis Ipsilateral cerebellar ataxia & HornerŌĆÖs syndrome
- 60. Vertebral artery stroke syndromes ŌĆó V1 & V4: Atherosclerotic lesion leads to low flow TIA(syncope, vertigo & alternating hemiplegia) ŌĆó V2&V3: dissection and fibromuscular dysplasia ŌĆó Lateral medullary and posterior inferior cerebellar infarct ŌĆó Embolic occlusion or thrombosis V4 leads lateral medullary syndrome ŌĆó Hemiparesis is not a feature of VA occlusion; however quadriparesis may result from anterior spinal artery occlusion
- 61. Vascular supply of medulla obolangata
- 62. Medial medullary infarct(face spare) Contralateral hemiparesis Most consistent Contralateral sensory impairment Contralateral lower limb and trunk, less often hand and arm Ipsilateral tongue weakness
- 63. Lateral Medullary syndrome Artery block: ICVA or PICA Vestibulo cerebellar symptoms and sign Contralateral spinothalamic sensory loss Ipsilateral facial pain: diagnostic of lateral tegmental brainstem localization Hiccough : dorsolateral middle medulla
- 64. Ipsilateral HornerŌĆÖs syndrome + ipsilateral ataxia +contralateral hypalgesia clinical triad of LMS Rostral medulla ’ü▒Severe dysphagia ’ü▒Hoarseness ’ü▒Facial paresis Caudal medulla ’üČMarked vertigo ’üČNystagmus ’üČGait disturbance
- 66. PICA cerebellar syndrome Vermis: medial PICA vertiginous labyrinthine syndrome: vertigo + nystagmus) Lateral cerebellar hemisphere PICA infarct: Acute unsteadiness with ataxia without vertigo or dysarthria Full PICA syndrome Ipsilateral occipitonuchal headache+ head tilt Vomiting, limb & gait ataxia, truncal lateralopulsion common Hypotonia rather than intention tremor is present
- 68. Hemimedullary syndrome (Reinhold syndrome) ŌĆó LMS + contralateral hemiparesis ŌĆó Block: occlusion of the ipsilateral vertebral artery proximal to the posterior inferior cerebellar artery and its anterior spinal artery branches
- 69. Distinguishing vertigo of brainstem and cerebellar from peripheral cause Three part HINTS (Head impulse Nystagmus test of skew) ŌĆó Most helpful in patient who have had continuous dizziness or vertigo ŌĆó HINTS is more sensitive than CT or MRI within first 2 days of onset of symptoms ŌĆó Abnormal test indicate peripheral vestibular lesion ŌĆó Except one caveat of AICA occlusion where HINTS test will be abnormal Suggest central vertigo ŌĆó Changing direction nystagmus ŌĆó normal head impulse test ŌĆó Skew deviation
- 70. Internal Carotid artery syndrome ACA MCA Anterior choroidal artery TMB may distinguish ICA from MCA syndrome Atherosclerotic narrowing Atherothrombotic occlusion Dissection
- 71. Anterior choroidal Artery stroke syndrome Invove structure Neurologic finding Posterior limb of internal capsule Contralateral hemiparesis Contralateral hemisensory loss LGB Affecting upper and lower field but sparing equator
- 72. Lateral geniculate body infarct Blood supply of LGB Quadriple sectoranopia
- 73. Subclavian artery disease ŌĆó Ipsilateral arm & hand symptoms ŌĆó Dizziness ŌĆó Visual symptoms ŌĆó Attacks are brief and brought on by exercising ischemic arm ŌĆó TakayasuŌĆÖs disease & GCA can cause subclavian and innominate artery disease ŌĆó Young women who smoke and taking OCP may develop occlusive disease
- 74. Innominate artery disease ŌĆó Monocular visual loss ŌĆó Cerebral ischemia (ACA+MCA) ŌĆó Arm ischemia ŌĆó Ischemic symptoms due to distal PCA & cerebellar symptoms
- 75. Cerebral venous sinus thrombosis ŌĆó Headache(90%), seizure (40%), raised ICP, stroke ŌĆó Hemorrhagic infarct that are not strictly arterial distribution ŌĆó SSST can causes para sagittal lesion ŌĆó MRV will demonstrate absence of signal
- 79. Vein of Galen thrombosis Stright sinus thrombosis Memory disturbance Diplopia Seizure Bithalamic infarct plus basal ganglia
- 80. Vein of Labe thrombosis The vein of Labbe, or inferior anastomotic vein, is part of the superficial central venous system and drains the temporal lobe and tissue adjacent to the Sylvian fissure. It connects the superficial middle cerebral vein draining into the transverse sinus
- 81. Cerebral small vessel disease ŌĆó Multifaceted cerebrovascular syndrome ŌĆó Distinct clinical, neuropathologic &neuroimaging presentation ’ü▒Small subcortical infarct ’ü▒Lacunes ’ü▒Cerebral microbleed(CMB) ’ü▒Cortical microinfarct ’ü▒Cortical superficial siderosis ’ü▒Enlarged perivascular space ’ü▒White matter hyperintensity (WMH) ’ü▒Brain atrophy Deep & superficial brain structure Isolated nerves , vasculature proper Stroke Dementia Gait disorder Incontinence Neuroimaging marker of small vessel disease
- 82. Take home message TMB gives clinical clue to ICA Arm symptoms may indicate subclavian or innominate artery disease Both ACA & MCA territory infarct may point towards ICA occlusion Basal ganglia involvement in imaging could help superficial & deep MCA occlusion Language can help to differentiate superior & inferior division MCA stroke Most PCA and MCA occlusion are embolic Border zone infarct point towards circulatory collapse and neck vessels stenosis