Venous eczema the prescriber's role
- 1. Venous Eczema – the prescriber’s role Linda Nazarko MSc, PgDip, PgCert, BSc(Hons), RN, NIP, OBE, FRCN Consultant Nurse West London Mental Health Trust Nurse Prescribing for Wound Care, ICO London 19 January 2016 ,
- 2. Aims and objectives To be aware of: ÔÅÆ Pathophysiology of venous disease ÔÅÆ Principles of diagnosis and treatment ÔÅÆ Diagnosis & treatment of venous eczema ÔÅÆ Diagnosis & treatment of infected venous eczema ÔÅÆ The topical steroids in managing flare ups, ÔÅÆ The role of emollient therapy ÔÅÆ Compression in maintaining skin health and comfort ÔÅÆ The value of the nurse practicing at advanced level.
- 3. Venous disease -pathophysiology ÔÅÆ Elevated venous pressure stretches and damages valves ÔÅÆ Valves fail, venous hypertension results ÔÅÆ Increased pressure superficial veins and capillaries
- 4. Prevalence & pre-disposing factors Venous disease affects 1/3 of adults. Predisposing factors: ÔÅÆ Abdominal tumour ÔÅÆ Ageing ÔÅÆ Obesity ÔÅÆ Pregnancy ÔÅÆ DVT
- 5. Ageing and the need for emollients Change Consequence Skin thins More easily damaged, increase risk of bruising and skin tears Replacement rate slows Takes longer to heal Reduced melanocytes Burns more easily Loss of collagen Saggy wrinkly skin Increased risk of skin tears, increased healing time, wounds more prone to breaking down Loss of fat Prominent veins, increased risk of bruising Reduced protective layer, increased risk of skin damage, increased risk of pressure sores. Loss of lipids and water Dry skin, cracks easily Increased risk of infection
- 6. What is venous eczema?  “A non infective inflammatory condition that affects the skin of the lower legs” (Gawkrodger, 2006).
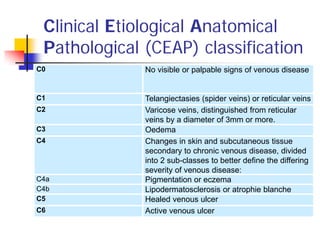
- 7. Clinical Etiological Anatomical Pathological (CEAP) classification C0 No visible or palpable signs of venous disease C1 Telangiectasies (spider veins) or reticular veins C2 Varicose veins, distinguished from reticular veins by a diameter of 3mm or more. C3 Oedema C4 Changes in skin and subcutaneous tissue secondary to chronic venous disease, divided into 2 sub-classes to better define the differing severity of venous disease: C4a Pigmentation or eczema C4b Lipodermatosclerosis or atrophie blanche C5 Healed venous ulcer C6 Active venous ulcer
- 8. Principles of diagnosis and treatment •This is a clinical diagnosisDiagnose venous eczema •Assess and treat symptoms, e.g infection, weeping, scale, red inflammed skin Treat eczema •Assess and check if safe to apply compression. If no contraindications apply compression Treat swelling •Obtain consent and refer for treatmentRefer for treatment of varicose veins •Advise on weight management, standing, walking, elevation and leg crossing Health promotion •Treat any issues affecting quality of life that have not been addressed such as pain Quality of life
- 9. Diagnosis of venous eczema ÔÅÆ Clinical diagnosis, use CEAP classification, observe for stigmata of venous disease ÔÅÆ Can lead to dry, thickened, scaly, cracked skin & can easily become infected
- 10. Diagnosis of infected venous eczema ÔÅÆ Check clinical features venous disease ÔÅÆ Check features of infection ÔÅÆ Check bloods, FBC, CRP, U&E ÔÅÆ Wound swab
- 11. Treatment of infected venous eczema  If systemic infection treat antibiotic therapy – local formulary usually flucloxacillin 500mg QDS if not penicillin allergic. Erythromycin or clindamycin if allergic.  Skin cleansing and debridment  Potassium permanganate soaks weeping eczema  Topically steroids and emollients
- 12. Potassium permanganate ÔÅÆ Astringent and antiseptic properties ÔÅÆ One tablet in 4 litres water = 1:10,000 solution on average 4 tablets her bucket. Line the bucket. Soak 10-15 minutes ÔÅÆ Use soft paraffin on nails to prevent staining ÔÅÆ Use for 3-5 days once or twice daily ÔÅÆ Store carefully ingestion can cause death through toxicity and organ failure
- 13. Infected venous eczema before & after ten days treatment
- 14. Treating red itchy inflamed skin -steroid therapy ÔÅÆ Eczema is a chronic inflammatory skin condition. The skin becomes red, inflamed, itchy and scaly (Steen, 2007: Holden & Berth-Jones, 2004). ÔÅÆ There are three stages of eczema: 1. Acute (when there is oozing, with tiny fluid filled lesions and swelling) 2. Subacute (scaly and red) 3. Chronic (thick and hyperpigmented skin ÔÅÆ Steroids can be used in acute and subacute stages.
- 15. Use of steroid therapy  Topical steroids classified according to potency  All (other than mild) can be used daily  Use for 14 days early discontinuation = relapse  Don’t use long term – thins skin  Use emollient therapy afterwards
- 16. Tips for prescribing and administering steroids ÔÅÆ The fingertip unit (FTU) is 0.5g of ointment and an adult lower leg requires three FTUs. ÔÅÆ Use moderately potent and potent steroids ÔÅÆ Apply steroids, leave to absorb and apply emollients 15-30 minutes after
- 17. Treating scale and lichenification ÔÅÆ Remove hyperkeratotic skin using Debrisoft pad or UCS debridement cloth ÔÅÆ Single treatment or 3-4 treatments
- 18. Why emollients are required ÔÅÆ Asteotic element to venous eczema, skin is dry ÔÅÆ Lipids restore normal barrier function and stop itching ÔÅÆ Reduces infection risk and flare ups
- 19. CKS guidance on emollients Consideration Recommendation Dryness of skin Mild to moderately dry use creams Moderate to severely dry – use ointments Weeping dermatitis Use creams as ointments will tend to slide off, becoming unacceptably messy. Frequency of application Creams are better tolerated but need to be applied more frequently and generously to have the same effect as a single application of ointment. Choice and acceptability Take account of the individual's preference, determined by the product's tolerability and convenience of use. Efficacy and acceptance Only a trial of treatment can determine if the individual finds a produce tolerable and convenient One size does not fit all More than one kind of product may be required. The intensity of treatment required and the area to be treated should guide treatment choice. Balancing acceptability and effectiveness The individual (and the prescriber) need to balance the effectiveness, tolerability and convenience of a product
- 21. Tips on emollient prescribing  Be generous – an adult can require 500g of emollient a week  Tailor prescribing to patient preference and ability to apply.  Beware of emollients containing lanolin – can cause sensitivity  Consider emollients with urea if skin unbroken  Be aware that patients can react to creams so monitor effect and change if concerns
- 22. Refer for treatment ÔÅÆ NICE guidance (2013) states that those with venous disease should be referred for assessment and treatment. ÔÅÆ Treatments include endothermal ablation, endovenous laser treatment of the long saphenous vein ultrasound guided foam sclerotherapy and surgery.
- 23. Treat the swelling  Compression bandages if severe  Compression stockings when settled  Elevate feet – higher than hip  Elevate foot of bed
- 24. Benefits of compression ÔÅÆ Reduces venous hypertension ÔÅÆ Reduces swelling ÔÅÆ Prevents ulceration ÔÅÆ Improves healing rates when ulceration occurs ÔÅÆ Improves comfort
- 25. NICE recommendations on compression ‘Do not offer compression hosiery to treat varicose veins unless interventional treatment is unsuitable.’ But: Patient may decline or not be well enough for surgery.
- 26. Bandages or stockings – the evidence  Mobile patients with highly exuding ulcers may require three or four layer bandaging (NICE, 2015: SIGN, 2010)  In all other cases two layer compression stockings are as effective as four layer compression bandaging (Ashby et al, 2013)  Its important to consult the patient and ensure that compression method meets his or her needs and aspirations
- 27. Assessment prior to compression ÔÅÆ Check for contraindications e.g severe heart failure ÔÅÆ Doppler ultrasound to check compression will not lead to compromised circulation ÔÅÆ Check condition of skin and debride if necessary
- 28. Hosiery selection Consult the patient  Thick, ribbed & sock like, for men and some ladies  Below knee  Above knee  Open and closed toe  Get the colour right  Grade two that is worn is better than grade three that isn’t.
- 29. Health promotion  Promote health  Weight loss if overweight  Don’t stand around for long periods  Activity - walking  Don’t cross legs  Don’t wear pop socks or socks that are tight at the top
- 30. Maintaining healthy skin  Use emollients  Protect skin from knocks  Don’t smoke  Protect skin from sun damage  Maintain good nutrition  Maintain hydration  Maintain health
- 31. Quality of life ÔÅÆ Venous disease can be horrible. The person may have dry itchy skin, weeping, infection, exudate, odour and swollen aching throbbing legs. ÔÅÆ A structured approach to management and treatment should address these issues but check. ÔÅÆ Address unresolved issues or refer
- 32. The value of advanced nursing practice ÔÅÆ Enables and empowers person to experience best possible quality of life. ÔÅÆ Treats problems promptly ÔÅÆ Prevents complications ÔÅÆ Enriches the lives of those we care for and our lives
- 33. Key points ÔÅÆ Venous disease is common in adults ÔÅÆ The prevalence of venous disease rises with age ÔÅÆ Changes caused by venous disease can lead to pain, discomfort and deteriorating health ÔÅÆ Lifestyle changes can improve well-being ÔÅÆ Effective management can treat complications and improve comfort. ÔÅÆ You can make a difference so use your diagnostic & prescribing skills.
- 34. Thank you for listening Any questions?