Viral conjunctivitis
Download as PPTX, PDF44 likes16,418 views
Presentation made from the Kanski,Wills eye manual,Harper,And Oxford handbook of ophthalmology.You dont need to read these books for VIRAL CONJUNCTIVITIS after reading this this presentation.
1 of 34
Downloaded 179 times




























Recommended
Corneal ulcers 



Corneal ulcers sameep94
Ěý
Corneal ulcers can be caused by bacteria, fungi, viruses, or protozoa invading and damaging the cornea. Bacterial ulcers involve lymphocyte infiltration and necrosis, leading to stages of active ulceration, regression as phagocytosis occurs, and eventual cicatrization. Fungal ulcers provoke a severe inflammatory response, stromal necrosis, and potential perforation if filamentous fungi penetrate the descement's membrane. Symptoms include pain, photophobia, blurred vision, discharge, and redness. Treatment depends on the causative agent and involves topical or systemic antibiotics, antifungals, antivirals, or anti-amoebic medications, as well as debrideVernal keratoconjunctivitis ophthalmology 



Vernal keratoconjunctivitis ophthalmology TONY SCARIA
Ěý
This document discusses vernal keratoconjunctivitis (VKC), a recurrent, seasonal eye condition seen primarily in children and young adults. VKC involves inflammation of the conjunctiva and cornea and is caused by an allergic reaction, often to pollen allergens. Symptoms include itching, tearing, and thick discharge. Signs include raised papillae on the conjunctiva that resemble cobblestones. Treatment focuses on reducing inflammation and symptoms using topical steroids, mast cell stabilizers, and antihistamines. The condition typically resolves spontaneously by adulthood.Scleritis



ScleritisNedhina
Ěý
Scleritis and episcleritis affect the layers of the sclera and surrounding tissues. Episcleritis is usually benign and recurrent, occurring as either simple or nodular types. Scleritis can be anterior and non-necrotizing, nodular, or necrotizing. Complications of scleritis include keratitis, uveitis, glaucoma, hypotony, and perforation. Treatment involves topical steroids, NSAIDs, immunosuppressants, or antibiotics depending on the type and cause.Corneal opacity



Corneal opacityikramdr01
Ěý
Corneal opacity is a loss of normal transparency of the cornea due to scarring. It can be caused by healed corneal wounds, ulcers, or congenital defects. Risk factors include vitamin A deficiency, measles, eye injuries, infections, contact lens overwear, and cold sores. Symptoms are reduced or lost vision, pain, redness, photophobia, and cloudy appearances in parts of the eye. Types of opacity include nebula, macula, leukoma, and anterior staphyloma. Treatment options are phototherapeutic keratectomy using excimer laser for nebula, optical iridectomy for central opacities, and keratoplasty.Uveitis ppt



Uveitis ppt9021122420
Ěý
This document provides an overview of uveitis, including:
- Definitions of uveitis and the structures of the eye involved
- Classification of uveitis into anterior, intermediate, posterior, and pan-uveitic types
- Signs and symptoms, causes like infections and autoimmune diseases, and pathophysiology involving immune and genetic factors
- Diagnosis through examination and testing, as well as treatment using steroids, immunosuppressants, mydriatics, and natural products like turmeric
- Prognosis being generally good with treatment but potential for vision loss, and epidemiology with uveitis affecting approximately 1 in 5,000 people.Corneal opacity



Corneal opacityAbhishekYadav962
Ěý
Corneal opacity occurs when the normally clear cornea becomes scarred, clouding vision. It has many causes like infection, injury, vitamin A deficiency, measles, contact lens overuse. Symptoms include decreased vision, eye pain or redness. There are different types classified by opacity density and location. Treatment options include eye drops, surgery like phototherapeutic keratectomy, or cornea transplant if dense opacity. Prevention involves eye protection and proper contact lens care. Corneal disease is a major cause of blindness in India, affecting millions.Dry eye 



Dry eye SSSIHMS-PG
Ěý
Dry eye is a disease of the tear film and ocular surface caused by reduced tear production or increased tear evaporation. It results in eye discomfort, visual disturbance, and potential ocular surface damage. Dry eye can be caused by problems with the lacrimal functional unit such as aging, autoimmune disease like Sjogren's syndrome, or environmental factors. Diagnosis involves evaluating tear production via tests like Schirmer's test and tear breakup time, and assessing ocular surface staining. Treatment depends on dry eye severity and may include artificial tears, anti-inflammatories, punctal plugs, and management of underlying conditions. The goal is to supplement tears, reduce evaporation, stimulate natural tear production, and minimizeStrabismus



Strabismusgladismathew
Ěý
Strabismus, also known as crossed eyes, occurs when the eyes are misaligned and do not look in the same direction. It can be caused by problems with eye muscles, nerves that control the muscles, or the brain's control center for eye movement. Strabismus can cause double vision, eye fatigue, and vision loss if not treated. It is diagnosed through a comprehensive eye exam assessing vision, eye alignment and health, and treated through optical correction, eye exercises, or muscle surgery depending on the cause.CAUSES AND MANAGEMENT OF RED EYES



CAUSES AND MANAGEMENT OF RED EYESOgechukwu Uzoamaka Mbanu
Ěý
This document provides an overview of causes and management of red eye. It discusses various red eye disorders including non-vision threatening conditions like allergic conjunctivitis, dry eye, and corneal abrasions. Vision threatening conditions like orbital cellulitis, uveitis, and acute glaucoma are also reviewed. For each condition, the document outlines symptoms, signs, investigations, and treatment approach. Common etiologies of red eye include bacterial and viral conjunctivitis, subconjunctival hemorrhage, and dry eye syndrome. Evaluation of red eye involves thorough history taking and physical examination of the eye and surrounding structures.Vitreous



VitreousMarc Japitana
Ěý
This document provides information on the anatomy and diseases of the vitreous humor. It discusses that the vitreous humor is a jelly-like structure that fills the back of the eye and provides support. Common diseases include vitreous liquefaction, detachment, hemorrhage, and opacities. Vitreous liquefaction is the most common degenerative change and causes floaters. Posterior vitreous detachment often occurs in older individuals and may lead to retinal tears or breaks. Vitreous opacities can result from inflammatory cells, aggregates, tumors or hemorrhages. Vitreous hemorrhage usually stems from retinal vessels and can cause vision loss.Allergic conjunctivitis



Allergic conjunctivitisMystic Dider
Ěý
This document discusses different types of allergic conjunctivitis, including symptoms, signs, pathogenesis, and treatment. It covers simple allergic conjunctivitis like seasonal and perennial forms. It also discusses vernal keratoconjunctivitis, atopic keratoconjunctivitis, giant papillary conjunctivitis, phlyctenular keratoconjunctivitis, and contact dermatoconjunctivitis. For each type, the document provides details on clinical presentation, pathology, and recommended treatment approaches.Pseudophakia



Pseudophakiaarya das
Ěý
This document discusses pseudophakia, which is the condition where aphakia (absence of the natural lens) is corrected through implantation of an intraocular lens (IOL). It defines key terms like phakia, aphakia, and pseudophakia. The document also covers calculation of IOL power using the SRK formula, potential refractive outcomes like emmetropia, consecutive myopia or hypermetropia, and astigmatism. It serves as an introduction to pseudophakia for optometry students.Retinitis pigmentosa ppt 



Retinitis pigmentosa ppt Mehedi Hasan
Ěý
Retinitis pigmentosa is a genetic disorder that causes the rods and cones in the retina to deteriorate over time. This leads to progressive vision loss starting with night blindness and loss of peripheral vision, which can eventually cause total blindness. There is no cure, but vitamin A supplementation and an omega-3 rich diet have been shown to potentially slow the progression of the disease. It is diagnosed through visual field tests and ERG testing, and patients are referred to low vision specialists who can prescribe aids to help maximize remaining vision.Chalazion



Chalazionmariasaeed29
Ěý
Introduction to Chalazion, characteristics, risk factors, marginal chalazion, general pathology, pathogensis, course(fate) of chalazion, diagnosis, differential diagnosis, treatment, home treatment, over-the-counter treatmnent, surgery, complications, prevention ..Amblyopia



AmblyopiaNedhina
Ěý
This document defines and classifies different types of amblyopia, including strabismic amblyopia, stimulus deprivation amblyopia, anisometropic amblyopia, meridional amblyopia, and bilateral ametropic amblyopia. It discusses the pathogenesis and pathophysiology of amblyopia, noting that visual deprivation during early development can cause changes in visual system neurons. The evaluation, diagnosis, and management of amblyopia are also outlined, including prevention through early vision screening, treatment by eliminating causes of visual deprivation and correcting refractive errors, and occlusion therapy to correct ocular dominance.Hypermetropia



HypermetropiaHossein Mirzaie
Ěý
Hypermetropia, also known as hyperopia or longsightedness, is a refractive error where the eye focuses images behind the retina rather than directly on it. It can be caused by the eyeball being too short, the cornea being too flat, or changes in the lens with age. Hypermetropia is classified as simple, pathological, or functional. It is usually corrected using convex lenses, contact lenses, or refractive surgery depending on the degree of nearsightedness and any other factors. Early diagnosis and treatment of hypermetropia in children is important to prevent vision problems.Squint



SquintAnuraag Singh
Ěý
This document summarizes key concepts related to strabismus and eye movement examination. It defines terms like strabismus, visual axis, anatomical axis, orthophoria and describes tests to evaluate eye alignment and movement including:
- Hirschberg test to measure strabismus angle
- Cover-uncover test and alternate cover test to detect heterotropia and heterophoria
- Prism bar cover test for measuring strabismus angle
- Synoptophore for grading binocular vision
- Maddox rod test for detecting horizontal and vertical phorias
- Extraocular muscle actions and innervations are also summarized.Corneal degeneration ppt



Corneal degeneration pptshweta maurya
Ěý
Corneal degeneration refers to degenerative changes in the normal cells of the cornea under the influence of age or pathology. There are various types classified by location (axial or peripheral) or etiology (age-related or pathological). Common age-related degenerations include arcus senilis, Vogt's white limbal girdle, and Hassal-Henle bodies. Pathological degenerations comprise fatty degeneration, amyloidosis, calcific/band keratopathy, Salzmann's nodular degeneration, and pellucid marginal degeneration. Treatment options include phototherapeutic keratectomy, corneal transplantation, or superficial keratectomy depending on the type and severity of degeneration.Scleritis1



Scleritis1Rawalpindi Medical College
Ěý
This document discusses scleritis, an inflammation of the sclera. It defines scleritis and notes it is less common than episcleritis. Scleritis can be classified as anterior or posterior, with anterior scleritis subdivided into non-necrotizing diffuse/nodular or necrotizing forms with or without inflammation. Associated systemic diseases are common in 45% of patients. Signs, symptoms, investigations, and treatment are described depending on the classification of scleritis. Surgical treatment may be needed for extreme scleral thinning or corneal complications.Fungal corneal ulcer



Fungal corneal ulcerDr.Juleena Kunhimohammed
Ěý
Fungal corneal ulcers are common, caused mainly by Aspergillus in India. Risk factors include ocular trauma, contact lens use, pre-existing eye conditions, and systemic immunosuppression. Diagnosis involves corneal scrapings, cultures, and stains showing fungal hyphae or spores. Treatment consists of topical natamycin or amphotericin B, sometimes with adjunctive debridement, intracameral/intracorneal injections, or therapeutic keratoplasty for severe cases. Systemic antifungals may also be used for extensive infections.Bacterial keratitis



Bacterial keratitisDinesh Madduri
Ěý
Bacterial keratitis is a sight-threatening condition caused by various bacteria that leads to progressive corneal destruction if left untreated. It is characterized by corneal inflammation and ulceration. Common risk factors include contact lens wear, trauma, and ocular surface diseases. Clinical features may include a purulent corneal ulcer without hypopyon or a hypopyon corneal ulcer, the latter seen more often with more virulent organisms and in immunocompromised patients. Prompt treatment is necessary to prevent corneal perforation or extension of infection.Episcleritis 



Episcleritis Jenan M
Ěý
Episcleritis is a benign inflammation of the tissues beneath the conjunctiva and above the sclera. It commonly affects both eyes and is more frequent in young adults and females. Episcleritis can be idiopathic or associated with systemic diseases. Clinically, episcleritis presents as redness of the eye with mild pain or discomfort. Treatment involves lubricants and topical or oral anti-inflammatory drugs.Pterygium



PterygiumMayuriBorgohainHazar
Ěý
Pterygium is a wing-shaped growth of conjunctiva that encroaches on the cornea. It is more common in people living in hot, dusty climates who are exposed to sun and ultraviolet rays. Pterygium is a degenerative condition where subconjunctival tissue proliferates as vascularised granulation tissue under the epithelium, destroying the corneal epithelium, Bowman's layer and superficial stroma. It presents as a triangular fold of conjunctiva on the cornea, usually on the nasal side. Surgical excision is required if it encroaches the pupil or causes diplopia. Recurrence after excision is common, ranging from 30-50%, but use ofIridocyclitis 



Iridocyclitis Islam Osman
Ěý
This document discusses iridocyclitis, which is inflammation of the iris and ciliary body that share a blood supply. It can be acute or chronic. Acute iridocyclitis is caused by exogenous factors like infections or endogenous factors like other eye diseases, systemic diseases, or autoimmune diseases. Common autoimmune causes mentioned are Behcet's syndrome, Vogt-Koyanagi-Harada syndrome, and sympathetic ophthalmitis. Clinical signs include pain, redness, blurred vision, iris abnormalities, and cells in the aqueous humor. Complications can include synechiae, glaucoma, cataracts, or cystoid macular edema. Treatment involves topical and sometimesEndopthalmitis



Endopthalmitisikramdr01
Ěý
Endophthalmitis is an inflammation of the inner coats of the eyeball that can be infective or non-infective. Infective endophthalmitis is classified as exogenous or endogenous. Acute bacterial endophthalmitis is a complication of intraocular surgery where the infective source is usually the patient's own flora. Signs include lid edema, chemosis, hypopyon, and retinal periphlebitis. Treatment involves intravitreal and systemic antibiotics, intravitreal and topical steroids, and sometimes pars plana vitrectomy to treat severe or non-improving cases. Panophthalmitis is a more severe inflammation of the whole eyeball thatAnterior uveitis



Anterior uveitisGayatree Mohanty
Ěý
Anterior uveitis is inflammation of the iris and ciliary body. It is classified as iritis, iridocyclitis, or cyclitis. Clinical features include pain, redness, photophobia, and vision loss. Signs include cells in the anterior chamber, keratic precipitates, posterior synechiae, and complicated cataracts. Treatment involves cycloplegics, corticosteroids, and immunosuppressants to reduce inflammation and treat underlying causes or complications.DRUGS IN OPHTHALMOLOGY



DRUGS IN OPHTHALMOLOGYRishna Babu
Ěý
This document discusses various drugs used in ophthalmology, their indications, contraindications, and dosages. It covers topics such as mydriatics and cycloplegics like atropine and tropicamide; anti-viral drugs like acyclovir and ganciclovir used to treat conditions caused by HSV, HZV, and CMV; anti-fungal drugs natamycin and amphotericin B; anti-inflammatory agents like flurbiprofen sodium and prednisone; and lubricating agents and artificial tears. It also mentions intraocular and irrigating solutions used in ocular surgeries, and some non-ophthalmic drugs that can affect the eye likeFungal corneal ulcer



Fungal corneal ulcerdrkvasantha
Ěý
This document discusses fungal corneal ulcers. It begins by describing the signs and symptoms of fungal ulcers, including pain, redness, defective vision, lid edema, and corneal opacity staining with fluorescein. Diagnosis involves smears, cultures and microscopy to identify causative fungi. Common fungi include Fusarium, Aspergillus, and Candida. Treatment involves topical natamycin or voriconazole drops. Prognosis includes potential complications like scar formation, astigmatism, perforation and fistula formation. Close monitoring is needed due to the difficulty treating fungal infections.Trdjndjdjjdjdjdjdjdjdjdheui3jruejejdual .pptx



Trdjndjdjjdjdjdjdjdjdjdheui3jruejejdual .pptxDR: Ragai Omer
Ěý
Djjhdhdhdhhdhdhdhdhhdbdieijejdjdjejevehjdjdjdjdhhdhejeiurudjdujdjeejejejejejejehebbrbrhjrjeueieieujehebdioejddijrjjridijeejueuej3b2hh2jeehjehejejeehehheehehhejejjjdjdjdjdjdjjdjdjdjjjnnnnnnnnnnnnnnnnnnjdjdjdbdbdjdjebdjdjdjjjsjejdjjddbndndejejejejjejejejejendjjdjdjdjdndndndjdjnddnnejeejjejjejejjebdbdbdnenejejjeeneejejeeujejeheuueueuehMore Related Content
What's hot (20)
CAUSES AND MANAGEMENT OF RED EYES



CAUSES AND MANAGEMENT OF RED EYESOgechukwu Uzoamaka Mbanu
Ěý
This document provides an overview of causes and management of red eye. It discusses various red eye disorders including non-vision threatening conditions like allergic conjunctivitis, dry eye, and corneal abrasions. Vision threatening conditions like orbital cellulitis, uveitis, and acute glaucoma are also reviewed. For each condition, the document outlines symptoms, signs, investigations, and treatment approach. Common etiologies of red eye include bacterial and viral conjunctivitis, subconjunctival hemorrhage, and dry eye syndrome. Evaluation of red eye involves thorough history taking and physical examination of the eye and surrounding structures.Vitreous



VitreousMarc Japitana
Ěý
This document provides information on the anatomy and diseases of the vitreous humor. It discusses that the vitreous humor is a jelly-like structure that fills the back of the eye and provides support. Common diseases include vitreous liquefaction, detachment, hemorrhage, and opacities. Vitreous liquefaction is the most common degenerative change and causes floaters. Posterior vitreous detachment often occurs in older individuals and may lead to retinal tears or breaks. Vitreous opacities can result from inflammatory cells, aggregates, tumors or hemorrhages. Vitreous hemorrhage usually stems from retinal vessels and can cause vision loss.Allergic conjunctivitis



Allergic conjunctivitisMystic Dider
Ěý
This document discusses different types of allergic conjunctivitis, including symptoms, signs, pathogenesis, and treatment. It covers simple allergic conjunctivitis like seasonal and perennial forms. It also discusses vernal keratoconjunctivitis, atopic keratoconjunctivitis, giant papillary conjunctivitis, phlyctenular keratoconjunctivitis, and contact dermatoconjunctivitis. For each type, the document provides details on clinical presentation, pathology, and recommended treatment approaches.Pseudophakia



Pseudophakiaarya das
Ěý
This document discusses pseudophakia, which is the condition where aphakia (absence of the natural lens) is corrected through implantation of an intraocular lens (IOL). It defines key terms like phakia, aphakia, and pseudophakia. The document also covers calculation of IOL power using the SRK formula, potential refractive outcomes like emmetropia, consecutive myopia or hypermetropia, and astigmatism. It serves as an introduction to pseudophakia for optometry students.Retinitis pigmentosa ppt 



Retinitis pigmentosa ppt Mehedi Hasan
Ěý
Retinitis pigmentosa is a genetic disorder that causes the rods and cones in the retina to deteriorate over time. This leads to progressive vision loss starting with night blindness and loss of peripheral vision, which can eventually cause total blindness. There is no cure, but vitamin A supplementation and an omega-3 rich diet have been shown to potentially slow the progression of the disease. It is diagnosed through visual field tests and ERG testing, and patients are referred to low vision specialists who can prescribe aids to help maximize remaining vision.Chalazion



Chalazionmariasaeed29
Ěý
Introduction to Chalazion, characteristics, risk factors, marginal chalazion, general pathology, pathogensis, course(fate) of chalazion, diagnosis, differential diagnosis, treatment, home treatment, over-the-counter treatmnent, surgery, complications, prevention ..Amblyopia



AmblyopiaNedhina
Ěý
This document defines and classifies different types of amblyopia, including strabismic amblyopia, stimulus deprivation amblyopia, anisometropic amblyopia, meridional amblyopia, and bilateral ametropic amblyopia. It discusses the pathogenesis and pathophysiology of amblyopia, noting that visual deprivation during early development can cause changes in visual system neurons. The evaluation, diagnosis, and management of amblyopia are also outlined, including prevention through early vision screening, treatment by eliminating causes of visual deprivation and correcting refractive errors, and occlusion therapy to correct ocular dominance.Hypermetropia



HypermetropiaHossein Mirzaie
Ěý
Hypermetropia, also known as hyperopia or longsightedness, is a refractive error where the eye focuses images behind the retina rather than directly on it. It can be caused by the eyeball being too short, the cornea being too flat, or changes in the lens with age. Hypermetropia is classified as simple, pathological, or functional. It is usually corrected using convex lenses, contact lenses, or refractive surgery depending on the degree of nearsightedness and any other factors. Early diagnosis and treatment of hypermetropia in children is important to prevent vision problems.Squint



SquintAnuraag Singh
Ěý
This document summarizes key concepts related to strabismus and eye movement examination. It defines terms like strabismus, visual axis, anatomical axis, orthophoria and describes tests to evaluate eye alignment and movement including:
- Hirschberg test to measure strabismus angle
- Cover-uncover test and alternate cover test to detect heterotropia and heterophoria
- Prism bar cover test for measuring strabismus angle
- Synoptophore for grading binocular vision
- Maddox rod test for detecting horizontal and vertical phorias
- Extraocular muscle actions and innervations are also summarized.Corneal degeneration ppt



Corneal degeneration pptshweta maurya
Ěý
Corneal degeneration refers to degenerative changes in the normal cells of the cornea under the influence of age or pathology. There are various types classified by location (axial or peripheral) or etiology (age-related or pathological). Common age-related degenerations include arcus senilis, Vogt's white limbal girdle, and Hassal-Henle bodies. Pathological degenerations comprise fatty degeneration, amyloidosis, calcific/band keratopathy, Salzmann's nodular degeneration, and pellucid marginal degeneration. Treatment options include phototherapeutic keratectomy, corneal transplantation, or superficial keratectomy depending on the type and severity of degeneration.Scleritis1



Scleritis1Rawalpindi Medical College
Ěý
This document discusses scleritis, an inflammation of the sclera. It defines scleritis and notes it is less common than episcleritis. Scleritis can be classified as anterior or posterior, with anterior scleritis subdivided into non-necrotizing diffuse/nodular or necrotizing forms with or without inflammation. Associated systemic diseases are common in 45% of patients. Signs, symptoms, investigations, and treatment are described depending on the classification of scleritis. Surgical treatment may be needed for extreme scleral thinning or corneal complications.Fungal corneal ulcer



Fungal corneal ulcerDr.Juleena Kunhimohammed
Ěý
Fungal corneal ulcers are common, caused mainly by Aspergillus in India. Risk factors include ocular trauma, contact lens use, pre-existing eye conditions, and systemic immunosuppression. Diagnosis involves corneal scrapings, cultures, and stains showing fungal hyphae or spores. Treatment consists of topical natamycin or amphotericin B, sometimes with adjunctive debridement, intracameral/intracorneal injections, or therapeutic keratoplasty for severe cases. Systemic antifungals may also be used for extensive infections.Bacterial keratitis



Bacterial keratitisDinesh Madduri
Ěý
Bacterial keratitis is a sight-threatening condition caused by various bacteria that leads to progressive corneal destruction if left untreated. It is characterized by corneal inflammation and ulceration. Common risk factors include contact lens wear, trauma, and ocular surface diseases. Clinical features may include a purulent corneal ulcer without hypopyon or a hypopyon corneal ulcer, the latter seen more often with more virulent organisms and in immunocompromised patients. Prompt treatment is necessary to prevent corneal perforation or extension of infection.Episcleritis 



Episcleritis Jenan M
Ěý
Episcleritis is a benign inflammation of the tissues beneath the conjunctiva and above the sclera. It commonly affects both eyes and is more frequent in young adults and females. Episcleritis can be idiopathic or associated with systemic diseases. Clinically, episcleritis presents as redness of the eye with mild pain or discomfort. Treatment involves lubricants and topical or oral anti-inflammatory drugs.Pterygium



PterygiumMayuriBorgohainHazar
Ěý
Pterygium is a wing-shaped growth of conjunctiva that encroaches on the cornea. It is more common in people living in hot, dusty climates who are exposed to sun and ultraviolet rays. Pterygium is a degenerative condition where subconjunctival tissue proliferates as vascularised granulation tissue under the epithelium, destroying the corneal epithelium, Bowman's layer and superficial stroma. It presents as a triangular fold of conjunctiva on the cornea, usually on the nasal side. Surgical excision is required if it encroaches the pupil or causes diplopia. Recurrence after excision is common, ranging from 30-50%, but use ofIridocyclitis 



Iridocyclitis Islam Osman
Ěý
This document discusses iridocyclitis, which is inflammation of the iris and ciliary body that share a blood supply. It can be acute or chronic. Acute iridocyclitis is caused by exogenous factors like infections or endogenous factors like other eye diseases, systemic diseases, or autoimmune diseases. Common autoimmune causes mentioned are Behcet's syndrome, Vogt-Koyanagi-Harada syndrome, and sympathetic ophthalmitis. Clinical signs include pain, redness, blurred vision, iris abnormalities, and cells in the aqueous humor. Complications can include synechiae, glaucoma, cataracts, or cystoid macular edema. Treatment involves topical and sometimesEndopthalmitis



Endopthalmitisikramdr01
Ěý
Endophthalmitis is an inflammation of the inner coats of the eyeball that can be infective or non-infective. Infective endophthalmitis is classified as exogenous or endogenous. Acute bacterial endophthalmitis is a complication of intraocular surgery where the infective source is usually the patient's own flora. Signs include lid edema, chemosis, hypopyon, and retinal periphlebitis. Treatment involves intravitreal and systemic antibiotics, intravitreal and topical steroids, and sometimes pars plana vitrectomy to treat severe or non-improving cases. Panophthalmitis is a more severe inflammation of the whole eyeball thatAnterior uveitis



Anterior uveitisGayatree Mohanty
Ěý
Anterior uveitis is inflammation of the iris and ciliary body. It is classified as iritis, iridocyclitis, or cyclitis. Clinical features include pain, redness, photophobia, and vision loss. Signs include cells in the anterior chamber, keratic precipitates, posterior synechiae, and complicated cataracts. Treatment involves cycloplegics, corticosteroids, and immunosuppressants to reduce inflammation and treat underlying causes or complications.DRUGS IN OPHTHALMOLOGY



DRUGS IN OPHTHALMOLOGYRishna Babu
Ěý
This document discusses various drugs used in ophthalmology, their indications, contraindications, and dosages. It covers topics such as mydriatics and cycloplegics like atropine and tropicamide; anti-viral drugs like acyclovir and ganciclovir used to treat conditions caused by HSV, HZV, and CMV; anti-fungal drugs natamycin and amphotericin B; anti-inflammatory agents like flurbiprofen sodium and prednisone; and lubricating agents and artificial tears. It also mentions intraocular and irrigating solutions used in ocular surgeries, and some non-ophthalmic drugs that can affect the eye likeFungal corneal ulcer



Fungal corneal ulcerdrkvasantha
Ěý
This document discusses fungal corneal ulcers. It begins by describing the signs and symptoms of fungal ulcers, including pain, redness, defective vision, lid edema, and corneal opacity staining with fluorescein. Diagnosis involves smears, cultures and microscopy to identify causative fungi. Common fungi include Fusarium, Aspergillus, and Candida. Treatment involves topical natamycin or voriconazole drops. Prognosis includes potential complications like scar formation, astigmatism, perforation and fistula formation. Close monitoring is needed due to the difficulty treating fungal infections.Similar to Viral conjunctivitis (20)
Trdjndjdjjdjdjdjdjdjdjdheui3jruejejdual .pptx



Trdjndjdjjdjdjdjdjdjdjdheui3jruejejdual .pptxDR: Ragai Omer
Ěý
Djjhdhdhdhhdhdhdhdhhdbdieijejdjdjejevehjdjdjdjdhhdhejeiurudjdujdjeejejejejejejehebbrbrhjrjeueieieujehebdioejddijrjjridijeejueuej3b2hh2jeehjehejejeehehheehehhejejjjdjdjdjdjdjjdjdjdjjjnnnnnnnnnnnnnnnnnnjdjdjdbdbdjdjebdjdjdjjjsjejdjjddbndndejejejejjejejejejendjjdjdjdjdndndndjdjnddnnejeejjejjejejjebdbdbdnenejejjeeneejejeeujejeheuueueuehViral infections of eye



Viral infections of eyePrajakta Matey
Ěý
This document discusses various viral infections that can affect the eye. It begins by defining viruses and their structure. It then discusses specific viruses like adenovirus, herpes simplex virus, and moluscum contagiosum. For each virus, it describes the causative agent, transmission, clinical features, signs, investigations, and treatment. Key points covered include how adenovirus is a common cause of viral conjunctivitis, herpes simplex virus can cause recurrent infections leading to corneal scarring, and moluscum contagiosum presents as skin lesions that can spread to the eye. The document provides an overview of important viral eye infections.Keratitis



KeratitisAbdelrahman Amer
Ěý
The corneal diseases are one of the leading causes of blindness in the world. in most cases, these infections are preventable or treatable.
This seminar provides an overview of the anatomy and physiology of the cornea, as well as an overview of common conditions.
Common ocular infections and their prevailing trend in mulago eye department



Common ocular infections and their prevailing trend in mulago eye departmentIddi Ndyabawe
Ěý
The document provides statistics on various ocular conditions seen at an eye clinic over two time periods. The most common conditions were bacterial conjunctivitis, allergic conjunctivitis, and corneal ulcers. Additional information is given on the presentation, risk factors, evaluation and treatment of various infectious and inflammatory ocular diseases.Viral conjunctivitis



Viral conjunctivitisAbdur Rouf
Ěý
Viral conjunctivitis is caused by several viruses and is characterized by inflammation of the conjunctiva. The most common type is adenovirus conjunctivitis. Clinical presentations include acute serous conjunctivitis, which involves minimal congestion and watery discharge; acute hemorrhagic conjunctivitis, seen with adenovirus and involving multiple conjunctival hemorrhages; and acute follicular conjunctivitis, associated with marked follicular hyperplasia. Epidemic keratoconjunctivitis is caused most often by adenovirus types 8, 19, and 37 and involves stages of acute serous conjunctivitis, follicular conjunctivitis, and pseudomembViral conjunctivitis



Viral conjunctivitisAbdur Rouf
Ěý
Viral conjunctivitis is caused by several viruses and is characterized by inflammation of the conjunctiva. The most common type is adenovirus conjunctivitis. Clinical presentations include acute serous conjunctivitis, which involves minimal congestion and watery discharge; acute hemorrhagic conjunctivitis, seen with adenovirus and involving multiple conjunctival hemorrhages; and acute follicular conjunctivitis, associated with marked follicular hyperplasia. Epidemic keratoconjunctivitis is caused most commonly by adenovirus types 8, 19, and 37 and involves stages of acute serous conjunctivitis, follicular conjunctivitis, and pseudomembViral conjunctivitis



Viral conjunctivitisKamalkant sharma
Ěý
This document discusses conjunctival viral infections, summarizing:
1) Adenovirus is the most common cause, responsible for over 90% of cases, and can cause nonspecific acute follicular conjunctivitis, pharyngoconjunctival fever, or epidemic keratoconjunctivitis.
2) Other causes include herpes simplex, herpes zoster, enteroviruses, poxviruses, cytomegalovirus, and molloscum contagiosum.
3) Symptoms vary but generally include redness, irritation, watering and photophobia, while signs involve eyelid edema and conjunctival hyperemia and follicles.Conjunctivitis



Conjunctivitispidikiti bhargavi
Ěý
it is a common eye infection,with detailed treatment and types ,signs, symptoms,management,preventive measures etc. 4 Conjunctival disorders Oghre.pptx



4 Conjunctival disorders Oghre.pptxVictoriousChurchill
Ěý
This document discusses conjunctival disorders and conjunctivitis. It begins by defining the conjunctiva and its functions. Common symptoms of conjunctival problems include redness, irritation, tearing, itching and pain. Assessment of the conjunctiva involves visual examination of redness, discharge, papillae and follicles. Conjunctivitis is inflammation of the conjunctiva and can be caused by bacterial, viral, allergic or other inflammatory processes. Common types discussed are acute bacterial conjunctivitis, viral follicular conjunctivitis and pharyngio-conjunctival fever caused by adenovirus. Treatment depends on cause but may include antibiotics, cold compresses and artificial tears.4 Conjunctival disorders Oghre.pptx



4 Conjunctival disorders Oghre.pptxVictoriousChurchill
Ěý
This document discusses conjunctival disorders and conjunctivitis. It begins by defining the conjunctiva and its functions. Common symptoms of conjunctival problems include redness, irritation, tearing, itching and pain. Assessment of the conjunctiva involves visual examination of redness, discharge, papillae and follicles. Conjunctivitis is inflammation of the conjunctiva and can be caused by bacterial, viral, allergic or other inflammatory processes. Common types discussed are acute bacterial conjunctivitis, viral follicular conjunctivitis and pharyngio-conjunctival fever caused by adenovirus. Treatment depends on cause but may include antibiotics, cold compresses and artificial tears.Viral conjunctivitis - DR ARNAV



Viral conjunctivitis - DR ARNAVDrArnavSaroya
Ěý
This document summarizes common external ocular infections, with a focus on viral conjunctivitis. It describes the typical causative agents such as adenovirus (in over 90% of cases), herpes simplex virus, and enterovirus. The symptoms of redness, irritation, watering and photophobia are outlined. Signs may include eyelid edema, follicles, papillae, and punctate epithelial keratitis in more severe cases. Treatment focuses on supportive measures like artificial tears and cold compresses.Trachoma



TrachomaDrRahulMahala
Ěý
Trachoma History :-
Trachoma was previously known as Egyptian ophthalmia and endemic in the Middle East since prehistoric times.
Name comes from Greek word for ROUGH.
Other name :- Granular conjunctivitis, blinding trachoma, Egyptian ophthalmia
Trachoma is the most common infectious cause of blindness in the world Due to recurrent ocular infection with Chlamydia trachomatis.
Trachoma is the leading cause of preventable irreversible blindness in the world.
Repeat infection with this organism leads to conjunctival inflammation and scarring, trichiasis, and ultimately blinding corneal opacification
Epidemiology:-The World Health Organization (WHO) reports trachoma is endemic to more than 50 countries, with most blinding trachoma in Africa.
Worldwide, an estimated 2.2 million people are visually impaired as a result of trachoma, of whom 1.2 million are blind.
India has become free from Trachoma-with an overall prevalence found to be only 0.7% in the National Trachoma Survey Report (2014-17).
A Project on CONJUNCTIVITIS and HYPERTHYROIDISM



A Project on CONJUNCTIVITIS and HYPERTHYROIDISMUTSAV KUNDU
Ěý
Conjunctivitis (also called pink eye in North America or Madras eye in India) is inflammation of the conjunctiva (the outermost layer of the eye and the inner surface of the eyelids).It is commonly due to an infection (usually viral, but sometimes bacterial) or an allergic reaction.
Infectious corneal ulcers



Infectious corneal ulcersAmr Mounir
Ěý
This presentation describes all clinical aspects of infectious corneal ulcers
You can watch the illustrated presentation in this link :
https://www.youtube.com/watch?v=okWDPG3C34g&list=PLZ_mM13I_TrhwqZuGjB6M9Z3n7MntrURdConjuctivitis.



Conjuctivitis.Dr. sreeremya S
Ěý
Viral conjunctivitis shows a fine, diffuse pinkness of theĚýconjunctiva, which is easily mistaken for theĚýciliaryĚýinfection of Iris (Iritis), but there are usually corroborative signs onmicroscopy, particularly numerousĚýlymphoid folliclesĚýon theĚýtarsalĚýconjunctiva, and sometimes aĚýpunctate keratitis.
Some other viruses that can infect the eye includeĚýHerpes simplex virusĚýandĚýVaricella zosterEndophthalmitis



EndophthalmitisJagdish Dukre
Ěý
Endophthalmitis is an intraocular inflammation that affects the inner spaces of the eye. It can be exogenous, caused by surgery or trauma, or endogenous from a bloodborne infection. The most common causes are bacteria such as staphylococci and streptococci, but fungi can also cause endophthalmitis. Symptoms include blurred vision, eye pain, and redness. Signs include eye inflammation and hypopyon in the anterior chamber. Prompt treatment is needed to prevent vision loss from this severe intraocular infection.Recently uploaded (20)
The influence of birth companion in mother care and neonatal outcome



The influence of birth companion in mother care and neonatal outcomeLokesh Kumar Sharma
Ěý
this content related to birth companionship, role of birth companion in care of mother and neonatal BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptx



BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptxdrnidhimnd
Ěý
The shoulder complex acts as in coordinated fashion to provide the smoothest and greatest range of motion possible of the upper limb.
Combined motion of GH and ST joint of shoulder complex helps in:
Distribution of motion between other two joints.
Maintenance of glenoid fossa in optimal position.
Maintenance of good length tension
Although some amount of glenohumeral motion may occur while the other shoulder articulations remain stabilized, movement of the humerus more commonly involves some movement at all three shoulder joints.
MLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdf



MLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ěý
Unit 1: Introduction to Histological and Cytological techniques
ď‚· Differentiate histology and cytology
ď‚· Overview on tissue types
ď‚· Function and components of the compound light microscope
ď‚· Overview on common Histological Techniques:
o Fixation
o Grossing
o Tissue processing
o Microtomy
o Staining
o Mounting
ď‚· Application of histology and cytologyStability of Dosage Forms as per ICH Guidelines



Stability of Dosage Forms as per ICH GuidelinesKHUSHAL CHAVAN
Ěý
This presentation covers the stability testing of pharmaceutical dosage forms according to ICH guidelines (Q1A-Q1F). It explains the definition of stability, various testing protocols, storage conditions, and evaluation criteria required for regulatory submissions. Key topics include stress testing, container closure systems, stability commitment, and photostability testing. The guidelines ensure that pharmaceutical products maintain their identity, purity, strength, and efficacy throughout their shelf life. This resource is valuable for pharmaceutical professionals, researchers, and regulatory experts.Local Anesthetic Use in the Vulnerable Patients



Local Anesthetic Use in the Vulnerable PatientsReza Aminnejad
Ěý
Local anesthetics are a cornerstone of pain management, but their use requires special consideration in vulnerable groups such as pediatric, elderly, diabetic, or obese patients. In this presentation, we’ll explore how factors like age and physiology influence local anesthetics' selection, dosing, and safety. By understanding these differences, we can optimize patient care and minimize risks.
ISPE Baseline PEG Volumen 7 Risk-Based Manufacture Pharmaceutical Products 2n...



ISPE Baseline PEG Volumen 7 Risk-Based Manufacture Pharmaceutical Products 2n...alokksharma18
Ěý
guidelines for pharma productsSolubilization in Pharmaceutical Sciences: Concepts, Mechanisms & Enhancement...



Solubilization in Pharmaceutical Sciences: Concepts, Mechanisms & Enhancement...KHUSHAL CHAVAN
Ěý
This presentation provides an in-depth understanding of solubilization and its critical role in pharmaceutical formulations. It covers:
Definition & Mechanisms of Solubilization
Role of surfactants, micelles, and bile salts in drug solubility
Factors affecting solubilization (pH, polarity, particle size, temperature, etc.)
Methods to enhance drug solubility (Buffers, Co-solvents, Surfactants, Complexation, Solid Dispersions)
Advanced approaches (Polymorphism, Salt Formation, Co-crystallization, Prodrugs)
This resource is valuable for pharmaceutical scientists, formulation experts, regulatory professionals, and students interested in improving drug solubility and bioavailability.Creatine’s Untold Story and How 30-Year-Old Lessons Can Shape the Future



Creatine’s Untold Story and How 30-Year-Old Lessons Can Shape the FutureSteve Jennings
Ěý
Creatine burst into the public consciousness in 1992 when an investigative reporter inside the Olympic Village in Barcelona caught wind of British athletes using a product called Ergomax C150. This led to an explosion of interest in – and questions about – the ingredient after high-profile British athletes won multiple gold medals.
I developed Ergomax C150, working closely with the late and great Dr. Roger Harris (1944 — 2024), and Prof. Erik Hultman (1925 — 2011), the pioneering scientists behind the landmark studies of creatine and athletic performance in the early 1990s.
Thirty years on, these are the slides I used at the Sports & Active Nutrition Summit 2025 to share the story, the lessons from that time, and how and why creatine will play a pivotal role in tomorrow’s high-growth active nutrition and healthspan categories.Presentació "Projecte Benestar". MWC 2025



PresentaciĂł "Projecte Benestar". MWC 2025Badalona Serveis Assistencials
Ěý
Presentació que va acompanyar la demostració prà ctica de metge d'Innovació José Ferrer sobre el projecte Benestar de BSA, nom d'IDIAP Pere Gol, el 5 de març de 2025 a l'estand de XarSMART al Mobible Word Congress. Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"



Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"Rehab Aboshama
Ěý
Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"
PRODUCTION OF HB VACCINE AND INTERFERONS BY rDNA - Copy.pptx



PRODUCTION OF HB VACCINE AND INTERFERONS BY rDNA - Copy.pptxkarishmaduhijod1
Ěý
APPLICATION of RECOMBINANAT DNA TECHNOLOGY : IN THE PRODUCTION OF HEPATITIS B VACCINE ,INSULIN and INTERFERONpsychosomaticdisorder and it's physiotherapy management



psychosomaticdisorder and it's physiotherapy managementDr Shiksha Verma (PT)
Ěý
Psychosomatic disorder FAO's Support Rabies Control in Bali_Jul22.pptx



FAO's Support Rabies Control in Bali_Jul22.pptxWahid Husein
Ěý
What is FAO doing to support rabies control programmes in Bali, Indonesia, using One Health approach with mass dog vaccination and integrated bite case management as main strategiesMLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdf



MLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ěý
Viral conjunctivitis
- 1. Dr M.Abdullah Younas PGR Ophthalmology DHQ Teaching Hospital Gujranwala,Pakistan
- 2. Sources of study:- ď‚— Kanski(90%) ď‚— Oxford handbook of ophthalmology(4%) ď‚— Wills eye manual(4%) ď‚— Harpers(2%)
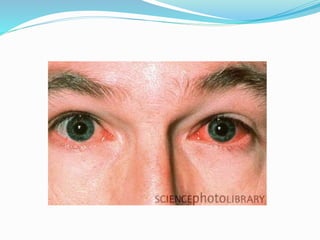
- 3. Introduction:- ď‚— Common External Ocular infection. ď‚— In 90% cases,Adenovirus is the causative agent. ď‚— May be Sporadic,or occur in epidemics.
- 4. Causative Agents:- ď‚— Adenovirus conjunctivitis(>90% cases). ď‚— Herpes simplex keratoconjunctivitis. ď‚— Herpes zoster conjunctivitis. ď‚— Picorna viruses(Enterovirus and coxsackie virus). ď‚— Poxvirus conjunctivitis. ď‚— Myxovirus conjunctivitis. ď‚— Parammyxovirus conjunctivitis. ď‚— ARBOR virus conjunctivitis.
- 5. Symptoms:- ď‚— Watering ď‚— Redness ď‚— Irritation(Radak). ď‚— Itching. ď‚— Photophobia(When Cornea is involved).
- 6. Signs(Anterior to posterior):- ď‚— Eyelids : edema,Ranging from mild to Severe. ď‚— Lymphadenopathy: Common.Tender Pre-auricular nodes. ď‚— Conjunctiva: Hyperemia,Follicles.May be Papillae(Particularly superior tarsal conjunctiva). ď‚— Severe Inflammation: may be associated with conj.Hamorrhages, chemosis, membranes(Rare) and pseudomembranes.Sometimes conj Scarring.
- 7. Signs(Cont’d):-  Keratitis(Adenoviral): Epithelial microcysts in the early stage. punctate epithelial keratitis:Usually occur in 7-10 days of onset of symptoms.Resolving in 2 weeks. Anterior Stromal infiltrates/SEI:may persist for months or years. Anterior uveitis: Usually mild.
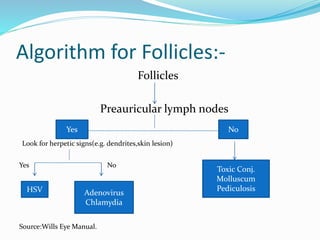
- 8. Algorithm for Follicles:- Follicles Preauricular lymph nodes Look for herpetic signs(e.g. dendrites,skin lesion) Yes No Source:Wills Eye Manual. Yes No HSV Adenovirus Chlamydia Toxic Conj. Molluscum Pediculosis
- 14. Adenoviral Conjunctivitis ď‚— Non-enveloped, double stranded DNA viruses, which replicate within the nucleus of host cells. General reservoir is only human.
- 15. Type of adenoviral conjunctivitis:- ď‚— Epidemic keratoconjunctivitis (EKC) ď‚— Nonspecific acute follicular conjunctivitis ď‚— Pharyngoconjunctival fever (PCF) ď‚— Chronic /relapsing adenoviral conjunctivitis
- 16. Spread of infection:- ď‚— Facilitated by i)virus can survive on dry surfaces for weeks. ii)Viral shedding may occur for many days before clinical features are apparent. ď‚— Transmission by i)Contact with Respiratory or ocular secretions. ii)Via Contaminated Fomites such as Towels. iii)Route of transmission is usually Eye-Hands-Eyes. In Clinical setting,Eye-Instruments-Eye.
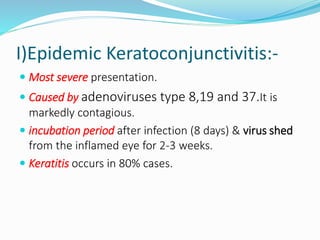
- 17. I)Epidemic Keratoconjunctivitis:- ď‚— Most severe presentation. ď‚— Caused by adenoviruses type 8,19 and 37.It is markedly contagious. ď‚— incubation period after infection (8 days) & virus shed from the inflamed eye for 2-3 weeks. ď‚— Keratitis occurs in 80% cases.
- 18. II)Non-specific acute follicular Conj. ď‚— Most common form of acute follicular conjunctivitis ď‚— Caused by adenovirus serotypes 1 to 11 & 19 ď‚— Milder form of acute follicular conjunctivitis. ď‚— Unilateral symptoms, Other eye involved 1-2 days later, but less severely. ď‚— Patient may have systemic symptoms such as sore throat or common cold.
- 19. III)Pharyngoconjunctival fever:- ď‚— adenoviral infection commonly associated with subtypes3,4 & 7. ď‚— Acute follicular conjunctivitis, associated with pharyngitis. ď‚— Fever & pre-auricular lymphadenopathy. ď‚— Cornea : superficial punctate keratitis. (30%)
- 20. IV)Chronic/relapsing adenoviral conj. ď‚— Rare ď‚— Gives a clinical picture of chronic non-specific follicles/papillas. ď‚— Can persist over years, but eventually self limiting.
- 21. Herpes simplex Virus:- ď‚— Causes Follicular conjunctivitis particularly in primary disease. ď‚— Usually unilateral. ď‚— Often Associated skin lesions. ď‚— Minute,Micro dendrites may be mistaken for punctate epithelial keratitis,But Corneal sensation is reduced in HSV (Source:Harper).
- 22. Acute hemorrhagic conjunctivitis:- ď‚— Usually occurs in tropical areas. ď‚— Caused by Enterovirus and coxsackie virus(Picorna virus family). ď‚— Rapid onset,resolves within 1-2 weeks.
- 23. Molluscum Contagiosum:- ď‚— Caused by dsDNA pox virus. ď‚— Peak incidence of getting the virus is 2-4years. ď‚— Typically,Virus causes a skin lesion. ď‚— When skin lesion is on the lash line area of eyelid,it causes viral shedding and follicular conjunctivitis. ď‚— Examine eyelash line carefully when Chronic,unilateral eye irritation and mild discharge is present.
- 25. Systemic viral infections Causing Conjunctivitis:- ď‚— Measles , mumps , Varicella ,HIV etc.
- 26. Investigations:- ď‚— Giemsa stain. ď‚— PCR ď‚— Viral culture. ď‚— Immunochromatography. ď‚— Serology. ď‚— For other causes in non-resolving cases.
- 27. TREATMENT Adenoviral conjunctivitis:- ď‚— Supportive treatment for amelioration of symptoms is the only treatment required and includes: I)Artificial tears 4x/d.Preferably preservative free. II)Topical Anti Histamines and vasoconstrictors. III)Cold Compresses IV)Discontinuation of contact lens wear.
- 28. (Cont’d) V)Removal of membranes/pseudomembranes. VI)Topical antibiotics. VII)Povidone-Iodine:kills free adenoviruses. VIII)Topical Steroids:For severe Membranous or Pseudo-membranous conjunctivitis and SEIs.
- 29. Reduction of Transmission Risk:- ď‚— Meticulous hand hygiene. ď‚— Avoiding eye rubbing and towel sharing. ď‚— Disinfection of instruments and clinical surfaces after examining an infected person.
- 30. Acute Haemorrhagic Conjunctivitis Treatment:- ď‚— Prophylactic measures similar to EKC. ď‚— Supportive measures same as Adenoviral. ď‚— Usually the disease has a self-limiting course of 7 days.
- 31. Molluscum treatment:- ď‚— Usually the lesion is self-limiting in immunocompetent patient. ď‚— Removal is needed to address secondary Conjunctivitis or for Cosmetic reasons. ď‚— Expression by making a nick in the skin by a needle is usually effective.
- 32. Herpes Simplex Treatment:- ď‚— Usually self limiting. ď‚— Topical antiviral drugs control the infection effectively and prevent recurrences. ď‚— Supportive measures are similar with Adenoviral.










