MANAGEMENT AND APPROACH OF (3).pptx
- 1. MANAGEMENT AND APPROACH TO A CHILD WITH HYPOGLYCEMIA BY DR FATIMA SHAFIQUE
- 2. ’éäOne of the major metabolic Emergencies at any age. ’éä Has potentially devastating Consequences on brain.
- 3. It is defined as serum blood glucose level < 55 mg/dl
- 5. THE BRAIN OF INFANT GROWS MOST RAPIDLY IN 1ST YEAR OF LIFE AND IT USES GLUCOSE AT RATE OF 4-6 MG/KG/MIN WHICH IS EQUAL TO ALL THE ENDOGENOUS PRODUCTION.
- 6. Glucose is also a source of ’éämembrane lipids, ’éäProtein synthesis ’éäprovides structural proteins and myelination imp for normal brain maturation.
- 7. Persistent Hypoglycemia Cerebral structural substrates are degraded Energy usable intermediates : lactate,pyruvate,amino acids,ketoacids Supports brain metabolism,at the expense of bain growth.
- 10. MANIFESTATION OF HYPOGLYCEMIA IN CHILDHOOD 1. Feature associated with activation of autonomic nervous system and epinephrine release ’éä Anxiety ŌĆĀ ’éä Perspiration ŌĆĀ ’éä Palpitation (tachycardia) ŌĆĀ ’éä Pallor ŌĆĪ ’éä Tremulousness ŌĆĪ ’éä Weakness ’éä Hunger ’éä Nausea ’éä Emesis
- 11. 2.Features associated with cerebral Glucopenia ’éä Headache ŌĆĀ ’éä Mental confusion ŌĆĀ ’éä Visual disturbances (Ōåō acuity, diplopia) ŌĆĀ ’éä Organic personality changes ŌĆĀ ’éä Inability to concentrate ŌĆĀ ’éä Dysarthria ’éä Staring ’éä Paresthesias ’éä Dizziness ’éä Amnesia ’éä Ataxia, incoordination ’éä Refusal to feed ŌĆĪ ’éä Somnolence, lethargy ŌĆĪ ’éä Seizures ŌĆĪ ’éä Coma
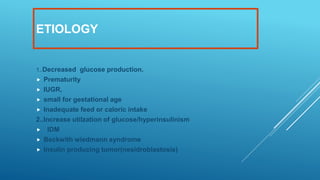
- 12. ETIOLOGY 1..Decreased glucose production. ’éä Prematurity ’éä IUGR, ’éä small for gestational age ’éä Inadequate feed or caloric intake 2..Increase utilzation of glucose/hyperinsulinism ’éä IDM ’éä Beckwith wiedmann syndrome ’éä Insulin producing tumor(nesidroblastosis)
- 13. Miscellaneous ’éä Sepsis ’éä Birth asphyxia ’éä Hypotermia ’éä Glycogen storage disease ’éä Glactosemia ’éä Hepatitis ’éä Maple syrup urine disease fatty acid oxidation defect ’éä Panhypopiturism ’éä Addison disease
- 14. CASE: A 1300 gram male baby is born via normal spontaneous vaignal delivery at 30 weeks gestation..mother is 29 years old with history of incompetent cervix. At delivery, the infant has a weak cry.not taking feed.and is pale and lethargic. His blood glucose is 30mg/dl.then he developed a seizure
- 15. ’ü« Hypoglycaemia in premature baby is common due to lack of Glycogen stores ,Decrease enzymatic activity (normaly decrease Glycogen synthase activity and rate limiting enzyme for gluconeogenesis phosphoenolpyruvate carboxykinase rise after birth) ’éä Inadequate substrates. ’éä Decrease muscle protein,body fat ’éä Decrease autonomic response
- 16. CASE: ’éä A newborn present witt jitteriness.his weight is 4kg Physical examination show a large plethoric infant who is tremulous. A murmer is heard blood sugar is low.(35mg/dl)mother had gestational diabetes during pregnancy
- 17. INFANT OF DIABETIC MOTHER (IDM) ’éä Pathophysiology. ’éä Maternal hypoglycemia cause fetal hyperglycemia and fetal pancreatic response lead to fetal hyperinsulinemia ’éä Fetal hyper insulinemia and hyperglycemia cause increase hepatic uptake of glucose... Accelerated lipogenesis and augmented protein synthesis so when separations of placenta at birth sudden interrupted glucose infusion without a proportional effect on hyperinsulinisn result in hypoglycemia
- 19. PERSISTENCE OR RECURRENT HYPOGLYCEMIA IN INFANT AND CHILDREN ’éä Hyperinsulinism is the most common cause of persistent hypoglycemia in early infancy. ’éä Infants who have hyperinsulinism may be macrosomic at birth, reflecting the anabolic effects of insulin in utero. ’éä There is no history or biochemical evidence of maternal diabetes. ’éäFactitious Hypoglycemia ’éä Hypoglycemia from exogenous administration of insulin as a form of child abuse.
- 23. ’éä measurement of serum IGFBP-1 concentration may help diagnose hyperinsulinism. The secretion of IGFBP-1 is acutely inhibited by insulin action; ’éä IGFBP-1 concentrations are low during hyperinsulinism- induced hypoglycemia. ’éä The differential diagnosis of endogenous hyperinsulinism includes Diffuse ╬▓-cell hyperplasia or focal ╬▓-cell microadenoma . ’éä The distinction between these 2 major entities is important because the diffuse hyperplasia, if unresponsive to medical therapy, requires near-total pancreatectomy
- 25. ISLET CELL ADENOMA ’éä Hyperinsulinemia as a result of islet cell adenoma should be considered in anychild Ōēź5 yr who presents with hypoglycemia. ’éä Islet cell adenomas do not ŌĆ£lightupŌĆØ during scanning with 18 F- labeled L -dopa. An islet cell adenoma in a child should arouse suspicion of the possibility of multiple endocrine neoplasia typeI (Wermer syndrome), which involves mutations in the menin gene and may be associated with hyperparathyroidism and pituitary tumors ’éä Islet cell adenomas at this age are treated by surgical excision.
- 27. CASE: ’éä A 36 week gestation infant was delivered weighing 3.9kg.He had an OMPHALOCELE and large tongue .there was no other abnormality observed. On laboratory investigations, there was hypoglycaemia.
- 30. CASE: ’éä A 6 year old child present with tiredness and weight loss for few weeks.There is blackening of skin colour due to generalised pigmentation.on laboratory investigations. Na is 118(hyponatremia),k 7.5(hyperkalemia) ..and hypoglycaemia. ACTH and renin level are raised
- 31. ADDISON'S DISEASE ’éä Acquired primary adrenal insufficiency originating in the gland itself..term addison disease.. ’éä Congenital adrenal hyperplasia ’éä Infection.. ’éä TB adrenalitis ’éä meningococcal sepsis or waterhouse friederichsen syndrome. ’éäSecondary cause ’éä Hypothalamic or pituitary tumor ’éä Due to Cortisol deficiency. Hypoglycemia that may associated with ketosis as body attempts to utilise fatty acid as alternative energy source
- 32. ’éäCase: ’éä A 9 month old boy present with sweating and tachypnea.on clincal examination, there is 5cm hepatomegaly.RBS is 40mg/dl.liver biopsy confirm Glycogen storage disease ’éä Type I Glucose-6-Phosphatase Deficiency ’éä Type III Glycogen Storage Disease(debrancher enzyme deficiancy) ’éä Liver Phosphorylase Deficiency (Type VI Glycogen Storage disease)
- 33. ’éä Diagnosis is made by simple investigation ’éä Blood gases thats show ’éä acidosis.. ’éä Hypoglycaemia ’éä Hyperuricemia ’éä Hyperlipidiemia ’éä G6PD is treated with a special diet in order to maintain normal glucose levels, prevent hypoglycemia and maximize growth and development. Frequent small servings of carbohydrates must be maintained during the day and night throughout the life. Calcium, vitamin D and iron supplements maybe recommended to avoid deficits.Uncooked corn starch.that are comlex carbs...are used
- 34. CASE: ’éä A 6 day old baby present with poor feeding and vomiting....LFT show hyperbillirubinemia..there is hypoglycaemia. Opthalmoloscopic examination central cataract .blood cultures are positive for E.Coli.he does well on intravenous fluids. when began on routine infant formula his symptoms return.
- 35. GLACTOCEMIA ’éä It is due to galactose 1 phosphate uridyl transferase deficiency.. ’éä Urine for reducing substance is positive..urine for ketone positive..direct enzyme activity in RBC is gold standard.. ’éä Management..avoiding all milk and milk containg products..and lactose free formula
- 36. CASE ’éä A 9 years old boy present with jaundice for last 10 days..now he has impaired consciousness. He has fever and vomiting. On examination, there is ascites and he is in coma.on investigation. There is hypoglycaemia and LFT are raised
- 37. ’éä Hepatic encephalopathy ’éä Investigation ’éä ..CBC ’éä LFT raised ’éä Conjugated hyperbilirubniema ’éä Metabolic profile .hypoglycemia ’éä Hypoalbunemia ’éä Hypokalemia ’éä Acid base disturbance
- 38. ’éä Frequent bedside monitoring of blood glucose every 2-4 hours. ’éä Severe hypoglycaemia is develop in majority of children..that lead to CNS impairments..so iv administration of glucose is required to prevent hypoglycaemia So prevention and management of hypoglycemia is important
- 40. ’éä Acute Presentation of symptoms: ’éä 1. Obtain blood sample before and 30 min after glucagon administration. ’éä 2. Obtain urine as soon as possible. Examine for ketones; if not present and hypoglycemia confirmed, suspect hyperinsulinemia or fatty acid oxidation defect; if present, suspect ketotic, hormone deficiency, inborn error of glycogen metabolism, or defective gluconeogenesis. ’éä 3. If glycemic increment after glucagon exceeds 40 mg/dL above basal,suspect hyperinsulinemia. ’éä 4. If insulin level at time of confirmed hypoglycemia is >5 ┬ĄU/mL, suspect endogenous hyperinsulinemia; if >100 ┬ĄU/mL, suspect factitious hyperinsulinemia (exogenous insulin injection). Admit to hospital for supervised fast. ’éä 5.If cortisol is <10 ┬Ąg/dL or growth hormone is <5 ng/mL, or both, suspect adrenal insufficiency or pituitary disease, or both. Admit to hospital forhormonal testing and neuroimaging.
- 42. Note: unusual behavior of any sick newborn should prompt a bedside glucose determination . ’éä However, because glucose meters have an accuracy of only ┬▒20%, any blood glucose value <60 mg/dL must be confirmed by a formal laboratory measurement that is performed without delay on a blood sample preserved in a tube that prevents glycolysis, which can cause spurious low values.