assisgnment.pptx
Download as PPTX, PDF0 likes12 views
this document thorough describes about juvenile arthritis types, signs and symptoms, epidemiology and treatment
1 of 22
Download to read offline





















Recommended
Arthritis



ArthritisShaza Kh
Ã˝
Pediatric rheumatoid arthritis is a form of arthritis that affects approximately 1 in 1,000 children each year. It involves inflammation of one or more joints and can cause pain, swelling, and stiffness. The most common types are juvenile rheumatoid arthritis and arthritis following a viral or bacterial infection. Treatment focuses on controlling inflammation through medications like DMARDs and biologics to prevent joint damage and disability. Nurses monitor for signs of arthritis, ensure proper treatment, educate patients and families, and help patients manage pain and maintain function.Juvenile Idiopathic Arthritis: diagnosis and treatment



Juvenile Idiopathic Arthritis: diagnosis and treatmentireskatsaniya
Ã˝
Juvenile idiopathic arthritis (JIA) is a chronic inflammatory disease that causes joint pain and swelling in children under 16 years old. It is the most common rheumatic disease in children. The cause is unknown but likely involves genetic and environmental factors. There are several subtypes of JIA classified by symptoms. Treatment aims to reduce inflammation and prevent joint damage through medications like NSAIDs, methotrexate, and biologics as well as physical and occupational therapy.SJIA- SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS.pptx



SJIA- SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS.pptxshekharyadv987
Ã˝
Detail study on Systemic juvenile idiopathic arthritis. Pediatric Rheumatic Diseases by JJ Laspoñas



Pediatric Rheumatic Diseases by JJ LaspoñasJJLasponas
Ã˝
Pediatric rheumatic diseases, also known as juvenile arthritis, are autoimmune and inflammatory conditions that affect nearly 300,000 children in the United States. They include conditions such as juvenile idiopathic arthritis, juvenile dermatomyositis, juvenile lupus, and juvenile scleroderma. Symptoms can include joint pain, swelling, stiffness, and fatigue. Diagnosis involves physical exams, medical history, and tests like ANA titers and RF tests. Treatment aims to relieve inflammation and control symptoms, with goals of improving comfort, managing pain, and maintaining mobility. Education of patients and families is important for effective self-management.juvenile Arthritis 



juvenile Arthritis pabitra sharma
Ã˝
Juvenile arthritis is a common condition in children that causes joint inflammation and pain. It can be classified as acute, sub-acute, or chronic based on the duration of symptoms. The most common type is juvenile idiopathic arthritis, which refers to conditions characterized by chronic joint inflammation. Treatment involves medications like NSAIDs and DMARDs to reduce inflammation and pain, physical or occupational therapy to maintain mobility, and surgery in severe cases to correct joint deformities. Nursing care focuses on alleviating pain, increasing mobility through exercise, promoting independence in self-care, and ensuring patients understand their condition and treatment plan.APPROACH TO A CHILD WITH ARTHRITIS-1.pptx



APPROACH TO A CHILD WITH ARTHRITIS-1.pptxEnohLena
Ã˝
Arthritis in a child: Approach for appropriate diagnosis and treatment: Presentation by SIMH ANDREAJIA clinical practice guidelines



JIA clinical practice guidelinesjuliann trumpower
Ã˝
This document provides clinical practice guidelines for the management of juvenile idiopathic arthritis (JIA). It discusses the background, epidemiology, risk factors, subtypes, clinical presentation, diagnostic studies, differential diagnosis, multidisciplinary management, medications, physical and occupational therapy, psychosocial interventions, complementary and alternative medicine, and implications for primary care providers of JIA. The goal of treatment is to control inflammation and pain, prevent morbidity and functional disability through a multidisciplinary approach including medications, physical therapy, and psychosocial support. Early recognition and treatment of JIA can positively impact outcomes.Rheumatoid arthritis, Educational Platform.pptx



Rheumatoid arthritis, Educational Platform.pptxnoorhadia494
Ã˝
This document provides an overview of rheumatoid arthritis, including its definition, signs and symptoms, causes, risk factors, complications, diagnosis, treatment, and nursing care. Rheumatoid arthritis is an autoimmune disorder where the immune system attacks joints, causing painful swelling. It most commonly affects adults over 50 and women. Smoking and excess weight can increase risk. Treatment focuses on reducing inflammation and symptoms through medications like NSAIDs, steroids, and disease-modifying drugs. Nurses assess patients, provide comfort measures, educate on disease management, and ensure patients can care for themselves.Juvenile_Idiopathic_Arthritis.pptx



Juvenile_Idiopathic_Arthritis.pptxazzaelnenaey
Ã˝
Juvenile Idiopathic Arthritis (JIA) is defined as arthritis of unknown cause that begins before age 16 and lasts over 6 weeks. It is classified based on symptoms into subtypes including systemic onset JIA, oligoarticular JIA, and polyarticular JIA. Treatment involves a stepwise approach starting with NSAIDs and intra-articular steroids and escalating to DMARDs and biologicals. Complications can include chronic anterior uveitis, osteoporosis, and potentially life-threatening macrophage activation syndrome.Rheumatoid arthritis.pptx



Rheumatoid arthritis.pptxHudaSaber1
Ã˝
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also affect other organs.
RA can occur at any age, but is more common in middle age. Women get RA more often than men.
Infection, genes, and hormone changes may be linked to the disease. Smoking may also be linked to RA.seronegative arthopathy



seronegative arthopathyBipulBorthakur
Ã˝
This document defines and describes seronegative spondyloarthropathy, a group of related inflammatory joint diseases that affect the spine. Key points:
- It refers to conditions where serological tests are typically negative for rheumatoid factor. The spine is commonly involved, starting in the sacroiliac joints.
- It includes ankylosing spondylitis, Reiter's syndrome, psoriatic arthritis, arthritis associated with inflammatory bowel disease, and undifferentiated spondyloarthropathies.
- Ankylosing spondylitis is the most common type and is associated with the HLA-B27 gene. It typically causes low back pain, morning stiffness, andRheumatoid arthritis nov 2020



Rheumatoid arthritis nov 2020Mukiza1
Ã˝
Rheumatoid arthritis is a chronic inflammatory disease that causes pain, stiffness, and swelling in the joints. It occurs when the immune system mistakenly attacks the joints, causing the synovial membrane to become inflamed. Over time, this can cause cartilage and bone damage and limit function. Treatment focuses on reducing inflammation, managing symptoms, and preventing further joint damage through medications, surgery, and lifestyle changes. While there is no cure, proper treatment can help improve quality of life by reducing pain and disability.Rheumatoid arthritis in infants topic.pdf



Rheumatoid arthritis in infants topic.pdfuzair23236565
Ã˝
This document provides an outline for a presentation on rheumatoid arthritis (RA) in infants. It covers key topics such as the challenges of diagnosing RA in infants given its non-specific symptoms, the importance of collaboration between specialists, and treatment considerations for these fragile patients. It also discusses juvenile idiopathic arthritis (JIA) more broadly, outlining its different subtypes and treatment goals and strategies. The conclusion emphasizes the resilience of infant patients and the need for further research to improve diagnosis, refine treatments, and ultimately pave the way for a brighter future with minimal disease impacts.Reactive arthritis



Reactive arthritisSachin Giri
Ã˝
This document discusses reactive arthritis (ReA), also known as Reiter's syndrome. It defines ReA as acute nonpurulent arthritis that occurs 1-4 weeks after an infection elsewhere in the body. Common infections that can trigger ReA include gastrointestinal or genitourinary infections by bacteria like Salmonella, Shigella, Yersinia, Campylobacter, or Chlamydia. The document discusses the pathophysiology, clinical features, diagnosis, treatment, and prevention of ReA. It also briefly summarizes some other systemic diseases that can present with arthritis symptoms, such as systemic lupus erythematosus, psoriatic arthritis, inflammatory bowel disease, rheumatic fever, andDr shridhar jia children and young people with arthritis.ppt



Dr shridhar jia children and young people with arthritis.pptmilanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments like DMARDS and biologicals, allowing for earlier diagnosis and tighter disease control to relieve pain, reduce inflammation, and preserve joint function. Effective treatment of JIA requires a multidisciplinary approach involving medical and therapy management.Dr shridhar jia children and young people with arthritis.ppt 121011



Dr shridhar jia children and young people with arthritis.ppt 121011milanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments, with an emphasis on early diagnosis and disease control to preserve joint function and normal development. Treatment is tailored differently for JIA compared to adult rheumatoid arthritis due to the involvement of a developing skeleton in children.Dr shridhar jia children and young people with arthritis



Dr shridhar jia children and young people with arthritismilanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments, with an emphasis on early diagnosis and disease control to preserve joint function and normal development. Treatment is tailored differently for JIA compared to adult rheumatoid arthritis due to the involvement of a developing skeleton in children.Dr shridhar jia children and young people with arthritis.ppt 121011



Dr shridhar jia children and young people with arthritis.ppt 121011milanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments like DMARDS and biologicals, allowing for earlier diagnosis and tighter disease control to relieve pain, reduce inflammation, and preserve joint function. Effective treatment of JIA requires a multidisciplinary approach.juvenile_rheumatoid_arthritis.ppt



juvenile_rheumatoid_arthritis.pptRitu32196
Ã˝
Juvenile Rheumatoid Arthritis (JRA) is an autoimmune disease that causes inflammation and damage to joints in children. It is classified based on the number and type of joints affected within the first 6 months. Treatment aims to suppress inflammation and involves NSAIDs, disease-modifying drugs like methotrexate, and glucocorticoids. Complications can include uveitis, growth impairment, and joint deformities. It is a multidisciplinary condition managed through pharmacological and non-pharmacological approaches.Ra conference may 2017



Ra conference may 2017Gregorio Cortes-Maisonet, MD, CHCP
Ã˝
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes inflammation of the joints. The document summarizes the definition, epidemiology, risk factors, pathophysiology, signs and symptoms, complications, diagnosis, and treatment of RA. It describes the clinical presentation of a patient with possible RA and the steps to take which include performing a physical exam, ordering diagnostic tests, making a provisional diagnosis, and referring the patient to a rheumatologist for further evaluation and management. Non-pharmacologic and pharmacologic treatment options for RA are outlined.Thyroid eye disease 



Thyroid eye disease AVURUCHUKWUNALUJAMES1
Ã˝
Thyroid eye disease (TED), also known as Graves' ophthalmopathy, is an autoimmune condition that affects the eyes and eyelids. It is commonly seen in patients with thyroid disease. The presentation can range from mild eyelid retraction to severe proptosis and optic neuropathy. The pathophysiology involves autoantibodies activating orbital fibroblasts and infiltrating lymphocytes, leading to inflammation and deposition of glycosaminoglycans in orbital tissues. Risk factors include smoking, female sex, and radioiodine treatment for hyperthyroidism. Clinical features depend on the stage of disease and can include dry eyes, eyelid swelling, proptosis, diplopia, and optic neuropathy. Classification systems consider soft tissueJuvenile idiopathic arthritis



Juvenile idiopathic arthritisAnas Bahnassi أنس البهنسي
Ã˝
This document discusses juvenile idiopathic arthritis (JIA), including its definition, signs and symptoms, patterns of onset, and treatment approaches. JIA is the most common rheumatic disease of childhood and can be divided into subtypes based on characteristics. Treatment involves NSAIDs initially and may progress to DMARDs like methotrexate or biological agents if needed. Management of uveitis associated with JIA relies on regular screening by an ophthalmologist and corticosteroid therapy if detected. The goal of JIA treatment is to minimize inflammation, control pain, preserve movement, and promote development.RHEUMATOLOGY(2).pptx



RHEUMATOLOGY(2).pptxSYEDZIYADFURQAN
Ã˝
Rheumatology deals with diseases of the joints, muscles, bones and tendons. The document discusses various types of arthritis including osteoarthritis, rheumatoid arthritis, pseudogout, gout and spondyloarthropathies. It covers the causes, risk factors, symptoms, investigations and treatment options for these conditions. Connective tissue diseases are also described which affect tissues between structures of the body. Management of arthritis in the elderly focuses on exercise, medications, assistive devices and lifestyle modifications.Rheumatoid arthritis and osteoarthritis presentation by Madhukar S Thagnar ....



Rheumatoid arthritis and osteoarthritis presentation by Madhukar S Thagnar ....MadhukarSureshThagna
Ã˝
Introduction
Risk factors
Sign and symptoms
Types of RA
Pathophysiology
Diagnosis
Treatment
Surgical management
Reference ATHRITIS Presentation, diqgnosis an.pptx



ATHRITIS Presentation, diqgnosis an.pptxokumuatanas1
Ã˝
Intended for health professional interested in renewing knowledge on arthritis.Seronegative Arthropathy.pptx



Seronegative Arthropathy.pptxJoydeep Tripathi
Ã˝
1. Seronegative spondyloarthritis is a group of inflammatory diseases characterized by inflammatory back pain, spinal and peripheral joint involvement, and enthesitis with a negative rheumatoid factor.
2. This family includes ankylosing spondylitis, psoriatic arthritis, enteropathic arthritis, reactive arthritis, and undifferentiated spondyloarthropathy.
3. Psoriatic arthritis is characterized by seronegative polysynovitis, erosive arthritis, enthesitis, dactylitis, and sacroiliitis or spondylitis. It commonly presents with distal interphalangeal joint involvement and nail changes.TIBIAL PLATEAU fracture power point presentation



TIBIAL PLATEAU fracture power point presentationKaliDereje
Ã˝
it explain about tibial plateau fracture and it medical management osteoarthritis of the hip and medical management .pdf



osteoarthritis of the hip and medical management .pdfKaliDereje
Ã˝
it explains in detail about hip osteoarthritis and its medical management More Related Content
Similar to assisgnment.pptx (20)
Rheumatoid arthritis, Educational Platform.pptx



Rheumatoid arthritis, Educational Platform.pptxnoorhadia494
Ã˝
This document provides an overview of rheumatoid arthritis, including its definition, signs and symptoms, causes, risk factors, complications, diagnosis, treatment, and nursing care. Rheumatoid arthritis is an autoimmune disorder where the immune system attacks joints, causing painful swelling. It most commonly affects adults over 50 and women. Smoking and excess weight can increase risk. Treatment focuses on reducing inflammation and symptoms through medications like NSAIDs, steroids, and disease-modifying drugs. Nurses assess patients, provide comfort measures, educate on disease management, and ensure patients can care for themselves.Juvenile_Idiopathic_Arthritis.pptx



Juvenile_Idiopathic_Arthritis.pptxazzaelnenaey
Ã˝
Juvenile Idiopathic Arthritis (JIA) is defined as arthritis of unknown cause that begins before age 16 and lasts over 6 weeks. It is classified based on symptoms into subtypes including systemic onset JIA, oligoarticular JIA, and polyarticular JIA. Treatment involves a stepwise approach starting with NSAIDs and intra-articular steroids and escalating to DMARDs and biologicals. Complications can include chronic anterior uveitis, osteoporosis, and potentially life-threatening macrophage activation syndrome.Rheumatoid arthritis.pptx



Rheumatoid arthritis.pptxHudaSaber1
Ã˝
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also affect other organs.
RA can occur at any age, but is more common in middle age. Women get RA more often than men.
Infection, genes, and hormone changes may be linked to the disease. Smoking may also be linked to RA.seronegative arthopathy



seronegative arthopathyBipulBorthakur
Ã˝
This document defines and describes seronegative spondyloarthropathy, a group of related inflammatory joint diseases that affect the spine. Key points:
- It refers to conditions where serological tests are typically negative for rheumatoid factor. The spine is commonly involved, starting in the sacroiliac joints.
- It includes ankylosing spondylitis, Reiter's syndrome, psoriatic arthritis, arthritis associated with inflammatory bowel disease, and undifferentiated spondyloarthropathies.
- Ankylosing spondylitis is the most common type and is associated with the HLA-B27 gene. It typically causes low back pain, morning stiffness, andRheumatoid arthritis nov 2020



Rheumatoid arthritis nov 2020Mukiza1
Ã˝
Rheumatoid arthritis is a chronic inflammatory disease that causes pain, stiffness, and swelling in the joints. It occurs when the immune system mistakenly attacks the joints, causing the synovial membrane to become inflamed. Over time, this can cause cartilage and bone damage and limit function. Treatment focuses on reducing inflammation, managing symptoms, and preventing further joint damage through medications, surgery, and lifestyle changes. While there is no cure, proper treatment can help improve quality of life by reducing pain and disability.Rheumatoid arthritis in infants topic.pdf



Rheumatoid arthritis in infants topic.pdfuzair23236565
Ã˝
This document provides an outline for a presentation on rheumatoid arthritis (RA) in infants. It covers key topics such as the challenges of diagnosing RA in infants given its non-specific symptoms, the importance of collaboration between specialists, and treatment considerations for these fragile patients. It also discusses juvenile idiopathic arthritis (JIA) more broadly, outlining its different subtypes and treatment goals and strategies. The conclusion emphasizes the resilience of infant patients and the need for further research to improve diagnosis, refine treatments, and ultimately pave the way for a brighter future with minimal disease impacts.Reactive arthritis



Reactive arthritisSachin Giri
Ã˝
This document discusses reactive arthritis (ReA), also known as Reiter's syndrome. It defines ReA as acute nonpurulent arthritis that occurs 1-4 weeks after an infection elsewhere in the body. Common infections that can trigger ReA include gastrointestinal or genitourinary infections by bacteria like Salmonella, Shigella, Yersinia, Campylobacter, or Chlamydia. The document discusses the pathophysiology, clinical features, diagnosis, treatment, and prevention of ReA. It also briefly summarizes some other systemic diseases that can present with arthritis symptoms, such as systemic lupus erythematosus, psoriatic arthritis, inflammatory bowel disease, rheumatic fever, andDr shridhar jia children and young people with arthritis.ppt



Dr shridhar jia children and young people with arthritis.pptmilanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments like DMARDS and biologicals, allowing for earlier diagnosis and tighter disease control to relieve pain, reduce inflammation, and preserve joint function. Effective treatment of JIA requires a multidisciplinary approach involving medical and therapy management.Dr shridhar jia children and young people with arthritis.ppt 121011



Dr shridhar jia children and young people with arthritis.ppt 121011milanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments, with an emphasis on early diagnosis and disease control to preserve joint function and normal development. Treatment is tailored differently for JIA compared to adult rheumatoid arthritis due to the involvement of a developing skeleton in children.Dr shridhar jia children and young people with arthritis



Dr shridhar jia children and young people with arthritismilanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments, with an emphasis on early diagnosis and disease control to preserve joint function and normal development. Treatment is tailored differently for JIA compared to adult rheumatoid arthritis due to the involvement of a developing skeleton in children.Dr shridhar jia children and young people with arthritis.ppt 121011



Dr shridhar jia children and young people with arthritis.ppt 121011milanb1
Ã˝
The document discusses juvenile idiopathic arthritis (JIA), the most common connective tissue disease in childhood. It notes that JIA is characterized by chronic arthritis lasting more than 6 weeks and presenting before age 16. The management of JIA has improved significantly with new drug treatments like DMARDS and biologicals, allowing for earlier diagnosis and tighter disease control to relieve pain, reduce inflammation, and preserve joint function. Effective treatment of JIA requires a multidisciplinary approach.juvenile_rheumatoid_arthritis.ppt



juvenile_rheumatoid_arthritis.pptRitu32196
Ã˝
Juvenile Rheumatoid Arthritis (JRA) is an autoimmune disease that causes inflammation and damage to joints in children. It is classified based on the number and type of joints affected within the first 6 months. Treatment aims to suppress inflammation and involves NSAIDs, disease-modifying drugs like methotrexate, and glucocorticoids. Complications can include uveitis, growth impairment, and joint deformities. It is a multidisciplinary condition managed through pharmacological and non-pharmacological approaches.Ra conference may 2017



Ra conference may 2017Gregorio Cortes-Maisonet, MD, CHCP
Ã˝
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes inflammation of the joints. The document summarizes the definition, epidemiology, risk factors, pathophysiology, signs and symptoms, complications, diagnosis, and treatment of RA. It describes the clinical presentation of a patient with possible RA and the steps to take which include performing a physical exam, ordering diagnostic tests, making a provisional diagnosis, and referring the patient to a rheumatologist for further evaluation and management. Non-pharmacologic and pharmacologic treatment options for RA are outlined.Thyroid eye disease 



Thyroid eye disease AVURUCHUKWUNALUJAMES1
Ã˝
Thyroid eye disease (TED), also known as Graves' ophthalmopathy, is an autoimmune condition that affects the eyes and eyelids. It is commonly seen in patients with thyroid disease. The presentation can range from mild eyelid retraction to severe proptosis and optic neuropathy. The pathophysiology involves autoantibodies activating orbital fibroblasts and infiltrating lymphocytes, leading to inflammation and deposition of glycosaminoglycans in orbital tissues. Risk factors include smoking, female sex, and radioiodine treatment for hyperthyroidism. Clinical features depend on the stage of disease and can include dry eyes, eyelid swelling, proptosis, diplopia, and optic neuropathy. Classification systems consider soft tissueJuvenile idiopathic arthritis



Juvenile idiopathic arthritisAnas Bahnassi أنس البهنسي
Ã˝
This document discusses juvenile idiopathic arthritis (JIA), including its definition, signs and symptoms, patterns of onset, and treatment approaches. JIA is the most common rheumatic disease of childhood and can be divided into subtypes based on characteristics. Treatment involves NSAIDs initially and may progress to DMARDs like methotrexate or biological agents if needed. Management of uveitis associated with JIA relies on regular screening by an ophthalmologist and corticosteroid therapy if detected. The goal of JIA treatment is to minimize inflammation, control pain, preserve movement, and promote development.RHEUMATOLOGY(2).pptx



RHEUMATOLOGY(2).pptxSYEDZIYADFURQAN
Ã˝
Rheumatology deals with diseases of the joints, muscles, bones and tendons. The document discusses various types of arthritis including osteoarthritis, rheumatoid arthritis, pseudogout, gout and spondyloarthropathies. It covers the causes, risk factors, symptoms, investigations and treatment options for these conditions. Connective tissue diseases are also described which affect tissues between structures of the body. Management of arthritis in the elderly focuses on exercise, medications, assistive devices and lifestyle modifications.Rheumatoid arthritis and osteoarthritis presentation by Madhukar S Thagnar ....



Rheumatoid arthritis and osteoarthritis presentation by Madhukar S Thagnar ....MadhukarSureshThagna
Ã˝
Introduction
Risk factors
Sign and symptoms
Types of RA
Pathophysiology
Diagnosis
Treatment
Surgical management
Reference ATHRITIS Presentation, diqgnosis an.pptx



ATHRITIS Presentation, diqgnosis an.pptxokumuatanas1
Ã˝
Intended for health professional interested in renewing knowledge on arthritis.Seronegative Arthropathy.pptx



Seronegative Arthropathy.pptxJoydeep Tripathi
Ã˝
1. Seronegative spondyloarthritis is a group of inflammatory diseases characterized by inflammatory back pain, spinal and peripheral joint involvement, and enthesitis with a negative rheumatoid factor.
2. This family includes ankylosing spondylitis, psoriatic arthritis, enteropathic arthritis, reactive arthritis, and undifferentiated spondyloarthropathy.
3. Psoriatic arthritis is characterized by seronegative polysynovitis, erosive arthritis, enthesitis, dactylitis, and sacroiliitis or spondylitis. It commonly presents with distal interphalangeal joint involvement and nail changes.Rheumatoid arthritis and osteoarthritis presentation by Madhukar S Thagnar ....



Rheumatoid arthritis and osteoarthritis presentation by Madhukar S Thagnar ....MadhukarSureshThagna
Ã˝
More from KaliDereje (15)
TIBIAL PLATEAU fracture power point presentation



TIBIAL PLATEAU fracture power point presentationKaliDereje
Ã˝
it explain about tibial plateau fracture and it medical management osteoarthritis of the hip and medical management .pdf



osteoarthritis of the hip and medical management .pdfKaliDereje
Ã˝
it explains in detail about hip osteoarthritis and its medical management knee osteoarthritis and physiotherapy management



knee osteoarthritis and physiotherapy managementKaliDereje
Ã˝
the power point thoroughly describes knee osteoarthritis and its physiotherapy management common muscle disorders .pptx



common muscle disorders .pptxKaliDereje
Ã˝
The document discusses common muscle disorders in pediatrics and contracture deformities. It covers several genetic muscle disorders including Duchenne muscular dystrophy, spinal muscular atrophy, and different types of muscular dystrophy. It then focuses on contracture deformities, defined as stiffness or constriction in connective tissues that limits range of motion. Common causes in children include inactivity, injury, burns, and genetic disorders like muscular dystrophy or cerebral palsy. Physiotherapy is a primary treatment using exercises and stretches to improve mobility and prevent further contractures.measurementsofmorbiditymortality-191120144157.pptx



measurementsofmorbiditymortality-191120144157.pptxKaliDereje
Ã˝
The document discusses various measurements used in epidemiology to measure mortality and morbidity. It defines key terms like incidence, prevalence, crude death rate, and standardized rates. It explains how to calculate different rates like crude death rate, specific death rate, case fatality rate, and proportional mortality rate. It also discusses the methods of direct standardization and indirect standardization to adjust rates. The learning objectives are to learn the basic measurements in epidemiology, how to select appropriate measurement tools, and how to measure and standardize mortality and morbidity rates.Fractures.pptx



Fractures.pptxKaliDereje
Ã˝
This power point contains fracture of the hand and shoulder. Additional to the fracture it has soft tissue injury of upper limb.CARBOHYDRATE 2023.pptx



CARBOHYDRATE 2023.pptxKaliDereje
Ã˝
This document provides information about basic nutrition and carbohydrates. It begins by outlining the objectives, which are to describe the functions of macronutrients, dietary fiber, and diseases associated with abnormal metabolisms. It then defines the six essential nutrients and explains that carbohydrates, proteins and fats are macronutrients that provide energy. Carbohydrates specifically are then discussed in more detail, including their classification, sources, and importance as the body's primary energy source. Overall, the document provides a high-level overview of basic nutrition with a focus on carbohydrates and their functions.CN disorder - Copy.ppt



CN disorder - Copy.pptKaliDereje
Ã˝
This document discusses cranial nerve disorders, nerve root lesions, nerve plexuses, and peripheral nerve lesions. It begins by covering trigeminal neuralgia, Bell's palsy, and cervical polyradiculopathy. For trigeminal neuralgia, the typical presentation, causes, diagnosis, and treatment including medications and microvascular decompression surgery are described. Bell's palsy is outlined as the most common type of facial paralysis. Cervical polyradiculopathy is then reviewed in terms of symptoms, common causes like spondylosis and disc herniation, evaluation, and initial treatment with conservative measures and epidural steroid injections.Anatomy of Muscular system.pdf



Anatomy of Muscular system.pdfKaliDereje
Ã˝
This document provides an overview of the muscular system. It discusses the basic functions of muscles including body movement, maintenance of posture, heat production, and controlling openings. It describes the properties of muscular tissue including excitability, contractibility, extensibility, and elasticity. It details the three types of muscles - skeletal, cardiac, and smooth muscle - and their characteristics. The document also covers muscle naming conventions, attachments, arrangements of fascicles, and examples of muscles in different body regions like the head, neck, abdomen, and arm.Anatomy Great blood vessels.pdf



Anatomy Great blood vessels.pdfKaliDereje
Ã˝
The document describes the major blood vessels in the human body. It discusses the structure and branches of the aorta, including the ascending aorta, aortic arch, and descending aorta. It also describes the major arteries and veins of the head, neck, upper limbs, thorax, abdomen, pelvis, and lower limbs. Additionally, it discusses arterial anastomoses, sites for compressing arteries to control bleeding, measuring blood pressure, thrombosis, and using saphenous veins for grafts.part ii.pptx



part ii.pptxKaliDereje
Ã˝
Clean the site with an alcohol swab in a circular motion from the center outward. Allow to air dry.
8. Put on sterile gloves
9. Pick up the needle and hold it like a dart. Insert the needle at 10-15 degree angle into the vein.
10. Advance the needle into the vein until blood flashes back into the hub.
11. Advance the catheter over the needle into the vein until resistance is felt.
12. Remove the needle and discard in a sharps container.
13. Attach the IV tubing to the catheter hub.
14. Release the tourniquet.
15. Secure the catheter to the skin using tape or transparent dressing.EMI assignment.pptx



EMI assignment.pptxKaliDereje
Ã˝
This document discusses electromagnetic induction and is divided into several sections. It introduces the group members and the topics to be covered, which include the history of electromagnetic induction, Faraday's law of induction, and Lenz's law of induction. Faraday discovered electromagnetic induction in 1831 through experiments showing that a changing magnetic field can induce an electromotive force in a conductor. Faraday's law states that the induced electromotive force is proportional to the rate of change of magnetic flux. Lenz's law explains that the induced current will flow in a direction to oppose the change that created it.disorders of veins.pptx



disorders of veins.pptxKaliDereje
Ã˝
This document discusses common disorders of arteries and veins, focusing on hypertensive vascular disease and atherosclerosis. It defines hypertension and outlines the pathogenesis of essential hypertension. Complications include stroke, heart disease, and renal failure. The document describes hyaline and hyperplastic arteriolosclerosis seen in hypertension. It also summarizes the risk factors, pathogenesis, and morphology of atherosclerosis, noting its role in cardiovascular diseases.electromagnetic induction



electromagnetic inductionKaliDereje
Ã˝
1. The document discusses electromagnetic induction and lists Faraday's laws of induction. It notes that electromagnetic induction is the phenomenon where electric current is generated by varying magnetic fields.
2. Faraday's first law states that an EMF is induced in a circuit whenever the magnetic flux through the circuit changes. The second law states that the magnitude of the induced EMF is directly proportional to the rate of change of the magnetic flux through the circuit.
3. Lenz's law explains that an induced current will flow in a direction to create a magnetic field that opposes the original changing magnetic field causing the induction.Cardiac and circulatory adaptation to exercise.pptx



Cardiac and circulatory adaptation to exercise.pptxKaliDereje
Ã˝
This document discusses the cardiovascular system and exercise. It begins with a list of group members and topics to discuss, including the functions of the cardiovascular system during exercise and long term effects of exercise. It then defines the cardiovascular system and describes how exercise places increased demands on the heart to pump more oxygen to working muscles. Key functions of the cardiovascular system during exercise are listed. Examples of aerobic physical activity and its benefits are provided. A list of popular cardiovascular exercises is given along with potential long term effects of regular exercise on the cardiovascular system, such as decreased resting heart rate and increased stroke volume.Recently uploaded (20)
Best Sampling Practices Webinar – USP <797> Compliance & Environmental Monito...



Best Sampling Practices Webinar – USP <797> Compliance & Environmental Monito...NuAire
Ã˝
Best Sampling Practices Webinar – USP <797> Compliance & Environmental Monitoring
Are your cleanroom sampling practices USP <797> compliant? This webinar, hosted by Pharmacy Purchasing & Products (PP&P Magazine) and sponsored by NuAire, features microbiology expert Abby Roth discussing best practices for surface & air sampling, data analysis, and compliance.
üí° Key Topics Covered:
✔️ Viable air & surface sampling best practices
✔️ USP <797> requirements & compliance strategies
✔️ How to analyze & trend viable sample data
✔️ Improving environmental monitoring in cleanrooms
üé• Watch Now: https://www.nuaire.com/resources/best-sampling-practices-cleanroom-usp-797
üì¢ Stay informed‚Äîfollow Abby Roth on LinkedIn for more cleanroom insights!ECZEMA 3rd year notes with images .pptx



ECZEMA 3rd year notes with images .pptxAyesha Fatima
Ã˝
If it’s not Itch It’s not Eczema
Eczema is a group of medical conditions which causes inflammation and irritation to skin.
It is also called as Dermatitis
Eczema is an itchy consisting of ill defined erythremotous patches. The skin surface is usually scaly and As time progress, constant scratching leads to thickened lichenified skin.
Several classifications of eczemas are available based on Etiology, Pattern and chronicity.
According to aetiology Eczema are classified as:
Endogenous eczema: Where constitutional factors predispose the patient to developing an eczema.
Family history (maternal h/o eczema) is often present
Strong genetic predisposition (Filaggrin gene mutations are often present).
Filaggrin is responsible for maintaining moisture in skin (hence all AD patients have dry skin.
Immunilogical factor-Th-2 disease, Type I hypersensitivity (hence serum IgE high)
e.g., Seborrheic dermatitis, Statis dermatitis, Nummular dermatitis, Dyshidrotic Eczema
Exogenous eczema: Where external stimuli trigger development of eczema,
e.g., Irritant dermatitis, Allergic Dermatitis, Neurodermatitis,
Combined eczema: When a combination of constitutional factors and extrinsic triggers are responsible for the development of eczema
e.g., Atopic dermatitis
Extremes of Temperature
Irritants : Soaps, Detergents, Shower gels, Bubble baths and water
Stress
Infection either bacterial or viral,
Bacterial infections caused by Staphylococcus aureus and Streptococcus species.
Viral infections such as Herpes Simplex, Molluscum Contagiosum
Contact allergens
Inhaled allergens
Airborne allergens
Allergens include
Metals eg. Nickle, Cobalt
Neomycin, Topical ointment
Fragrance ingredients such as Balsam of Peru
Rubber compounds
Hair dyes for example p-Phenylediamine
Plants eg. Poison ivy .
Atopic Dermatitis : AD is a chronic, pruritic inflammatory skin disease characterized by itchy inflamed skin.
Allergic Dermatitis: A red itchy weepy reaction where the skin has come in contact with a substance That immune system recognizes as foreign substances.
Ex: Poison envy, Preservatives from creams and lotions.
Contact Irritant Dermatitis: A Localized reaction that include redness, itching and burning where the skin has come In contact with an allergen or with irritant such as acid, cleaning agent or chemical.
Dyshidrotic Eczema: Irritation of skin on the palms and soles by
clear deep blisters that itch and burn.
Clinical Features; Acute Eczema:- Acute eczema is characterized by an erythematous and edematous plaque, which is ill-defined and is surmounted by papules, vesicles, pustules and exudate that dries to form crusts. A subsiding eczematous plaque may be covered with scales.
Chronic Eczema:- Chronic eczema is characterized by lichenification, which is a triad of hyperpigmentation, thickening markings. The lesions are less exudative and more scaly. Flexural lesions may develop fissures.
Pruritus
Characteristic Rash
Chronic or repeatedly occurring symptoms.SAPIENT Medi-trivia Quiz (FINALS) | TRI-ORTA 2025



SAPIENT Medi-trivia Quiz (FINALS) | TRI-ORTA 2025Dr. Anindya
Ã˝
Final Round of SAPIENT Medi-trivia quiz
Part of TRI-ORTA 2025
Venue: GLT, Medical College Kolkata
Date: 25-02-2025Macafem Reviews 2024 - Macafem for Menopause Symptoms



Macafem Reviews 2024 - Macafem for Menopause SymptomsMacafem Supplement
Ã˝
At Macafem, we provide 100% natural support for women navigating menopause. For over 20 years, we've helped women manage symptoms, and in 2024, we're proud to share their heartfelt experiences.X-Ray-Generators-and-Transformers final.pdf



X-Ray-Generators-and-Transformers final.pdfMohd Faraz
Ã˝
An X-ray generator is a crucial device used in medical imaging, industry, and research to produce X-rays. It operates by accelerating electrons toward a metal target, generating X-ray radiation. Key components include the X-ray tube, transformer assembly, rectifier system, and high-tension circuits. Various types, such as single-phase, three-phase, constant potential, and high-frequency generators, offer different efficiency levels. High-frequency generators are the most advanced, providing stable, high-quality imaging with minimal radiation exposure. X-ray generators play a vital role in diagnostics, security screening, and industrial testing while requiring strict radiation safety measures.Sudurpaschim logsewa aayog Medical Officer 8th Level Curriculum



Sudurpaschim logsewa aayog Medical Officer 8th Level CurriculumDr Ovels
Ã˝
Sudurpaschim province psc ( lok sewa aayog) medical officer 8th level syllabusFlag Screening in Physiotherapy Examination.pptx



Flag Screening in Physiotherapy Examination.pptxBALAJI SOMA
Ã˝
Flag screening is a crucial part of physiotherapy assessment that helps in identifying medical, psychological, occupational, and social barriers to recovery. Recognizing these flags ensures that physiotherapists make informed decisions, provide holistic care, and refer patients appropriately when necessary. By integrating flag screening into practice, physiotherapists can optimize patient outcomes and prevent chronicity of conditions.MALE REPRODUCTIVE PHYSIOLOGY up load.pptx



MALE REPRODUCTIVE PHYSIOLOGY up load.pptxYIHENEW CHALLIE LIYEW
Ã˝
Male animal reproductive physiology including sexual maturity ,reproductive hormone ,sperm production Optimization in Pharmaceutical Formulations: Concepts, Methods & Applications



Optimization in Pharmaceutical Formulations: Concepts, Methods & ApplicationsKHUSHAL CHAVAN
Ã˝
This presentation provides a comprehensive overview of optimization in pharmaceutical formulations. It explains the concept of optimization, different types of optimization problems (constrained and unconstrained), and the mathematical principles behind formulation development. Key topics include:
Methods for optimization (Sequential Simplex Method, Classical Mathematical Methods)
Statistical analysis in optimization (Mean, Standard Deviation, Regression, Hypothesis Testing)
Factorial Design & Quality by Design (QbD) for process improvement
Applications of optimization in drug formulation
This resource is beneficial for pharmaceutical scientists, R&D professionals, regulatory experts, and students looking to understand pharmaceutical process optimization and quality by design approaches.BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptx



BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptxdrnidhimnd
Ã˝
The shoulder complex acts as in coordinated fashion to provide the smoothest and greatest range of motion possible of the upper limb.
Combined motion of GH and ST joint of shoulder complex helps in:
Distribution of motion between other two joints.
Maintenance of glenoid fossa in optimal position.
Maintenance of good length tension
Although some amount of glenohumeral motion may occur while the other shoulder articulations remain stabilized, movement of the humerus more commonly involves some movement at all three shoulder joints.
HUMAN SEXUALITY AND SEXUAL RESPONCE CYCLE



HUMAN SEXUALITY AND SEXUAL RESPONCE CYCLEdaminipatel37
Ã˝
It is all about topic of obg for new semester students Non-Invasive ICP Monitoring for Neurosurgeons



Non-Invasive ICP Monitoring for NeurosurgeonsDhaval Shukla
Ã˝
This presentation delves into the latest advancements in non-invasive intracranial pressure (ICP) monitoring techniques, specifically tailored for neurosurgeons. It covers the importance of ICP monitoring in clinical practice, explores various non-invasive methods, and discusses their accuracy, reliability, and clinical applications. Attendees will gain insights into the benefits of non-invasive approaches over traditional invasive methods, including reduced risk of complications and improved patient outcomes. This comprehensive overview is designed to enhance the knowledge and skills of neurosurgeons in managing patients with neurological conditions.
Invasive systems are commonly used for monitoring intracranial pressure (ICP) in traumatic brain injury (TBI) and are considered the gold standard. The availability of invasive ICP monitoring is heterogeneous, and in low- and middle-income settings, these systems are not routinely employed due to high cost or limited accessibility. The aim of this presentation is to develop recommendations to guide monitoring and ICP-driven therapies in TBI using non-invasive ICP (nICP) systems.
Asthma: Causes, Types, Symptoms & Management – A Comprehensive Overview



Asthma: Causes, Types, Symptoms & Management – A Comprehensive OverviewDr Aman Suresh Tharayil
Ã˝
This presentation provides a detailed yet concise overview of Asthma, a chronic inflammatory disease of the airways. It covers the definition, etiology (causes), different types, signs & symptoms, and common triggers of asthma. The content highlights both allergic (extrinsic) and non-allergic (intrinsic) asthma, along with specific forms like exercise-induced, occupational, drug-induced, and nocturnal asthma.
Whether you are a healthcare professional, student, or someone looking to understand asthma better, this presentation offers valuable insights into the condition and its management.assisgnment.pptx
- 2. OUTLINE • Introduction • Definition and Types • Epidemiology • Etiology and Risk Factors • Signs and Symptoms • Diagnosis • Treatment • Complications and Prognosis • Physiotherapy Treatment of Juvenile Arthritis • Conclusion
- 3. Juvenile arthritis • is a chronic autoimmune condition that affects children and adolescents under the age of 16. • It is characterized by joint inflammation, pain, and stiffness, which can lead to long-term disability if left untreated. • JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs.
- 4. • Juvenile arthritis is a broad term that encompasses several subtypes of arthritis that occur in children. • The most common form is called juvenile idiopathic arthritis (JIA), previously known as juvenile rheumatoid arthritis (JRA).
- 5. Epidemiology • JIA is the most common chronic heterogenous rheumatologic condition in children. • It is estimated that around 3 million children and young adults have JIA. The global prevalence is believed to range from 3.8 to 400/100,000; the incidence is estimated to be 1.6 to 23/100,000. • Females are at higher risk of JIA than males. • The oligoarticular subtype is more common. 5
- 6. ETIOLOGY • The exact cause of juvenile arthritis is unknown. • a combination of  genetic, a role, as certain genes have been associated with an increased risk of developing the disease. environmental, immunological factors, dysregulation of the immune system, specifically autoimmunity.
- 7. RISK FACTORS • A family history of autoimmune diseases • Genetic • Exposure to infections or other environmental triggers • Females
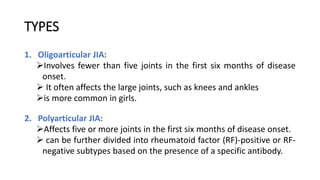
- 8. TYPES 1. Oligoarticular JIA: ÔÉòInvolves fewer than five joints in the first six months of disease onset. ÔÉò It often affects the large joints, such as knees and ankles ÔÉòis more common in girls. 2. Polyarticular JIA: ÔÉòAffects five or more joints in the first six months of disease onset. ÔÉò can be further divided into rheumatoid factor (RF)-positive or RF- negative subtypes based on the presence of a specific antibody.
- 9. 3. Systemic JIA: ÔÉòInvolves inflammation in one or more joints, along with systemic symptoms such as high fever, rash, and generalized enlargement of lymph nodes. 4. Enthesitis-related arthritis: ÔÉòInflammation occurs at the sites where tendons and ligaments attach to bones (entheses). ÔÉòIt is often associated with enthesitis, arthritis, and enthesopathy.
- 10. 5. Psoriatic arthritis: ÔÉòPresents with both joint inflammation and skin manifestations, such as psoriasis or nail changes. 6. Other rare subtypes: ÔÉòThese include juvenile lupus, juvenile dermatomyositis, and juvenile spondyloarthropathies
- 12. SIGN AND SYMPTOMS • The signs and symptoms of juvenile arthritis vary depending on the subtype and the individual child. Common features include:  Joint pain: Persistent pain in one or more joints, which may be worse in the morning or after periods of rest.  Joint swelling: Affected joints may appear swollen, warm to the touch, and tender.  Joint stiffness: Stiffness and limited range of motion in the affected joints, especially upon waking up in the morning or after periods of inactivity.
- 13.  Fatigue: Generalized tiredness and lack of energy, which can affect a child's daily activities.  Systemic symptoms: Systemic JIA may present with high spiking fevers, rash, and enlarged lymph nodes.  Eye inflammation: Certain subtypes of juvenile arthritis, such as oligoarticular JIA, can be associated with uveitis, an inflammation of the eye. • It is important to note that the symptoms may fluctuate in severity, with periods of flare-ups and remission.
- 14. • The diagnosis is typically based on a combination of clinical findings, medical history, physical examination, and laboratory tests. • Laboratory tests commonly used in the diagnostic process include:  Blood tests: such as CBC, ESR, CRP, RF, and ANA testing. These tests help assess the presence of inflammation and autoimmune markers.  Joint fluid analysis:  Imaging studies: X-rays and other imaging modalities, such as US and MRI. Eye examination
- 15. TREATMENT • The management of juvenile arthritis aims to control symptoms, prevent joint damage, and improve the child's quality of life. • Treatment plans are individualized based on the subtype, disease activity, and the child's specific needs. • A multidisciplinary approach involving rheumatologists, physical therapists, occupational therapists, and other healthcare professionals is often necessary.
- 16. • Treatment options for juvenile arthritis include:  Nonsteroidal anti-inflammatory drugs (NSAIDs):  Disease-modifying antirheumatic drugs (DMARDs):  Biologic agents:  Corticosteroids
- 17. COMPLICATION • Without appropriate treatment, juvenile arthritis can lead to significant complications and long-term disability such as  Joint damage,  deformities, and  growth disturbances are possible outcomes, particularly if the disease remains uncontrolled. • Children with systemic JIA may experience complications related to systemic inflammation, such as pericarditis or macrophage activation syndrome.
- 18. PROGNOSIS • The prognosis for juvenile arthritis varies depending on the subtype, disease severity, and the child's response to treatment. • Early diagnosis and prompt initiation of appropriate therapy are associated with better outcomes. • Regular follow-up with a rheumatologist is essential to monitor disease activity, adjust treatment as needed, and address any emerging complications.
- 19. PHYSIOTHERAPY ASSESSMENT • Assessment include a thorough examination of  joint range of motion,  muscle strength,  posture, and  functional abilities. • It helps the physiotherapist develop an individualized treatment plan tailored to the child's specific needs
- 20. • Aim of physiotherapy management  to reduce the pain  to improve joint mobility and ROM  to improve the muscle strength and balance  to improve posture and alignment  to achieve functional independence  to promotes physical fitness  patient education
- 21. • Physiotherapy management include  ROM exercises  Strengthening Exercises  Heat therapy  Cold therapy  Transcutaneous electrical nerve stimulation (TENS)
- 22. ÔÉò Ultrasound therapy ÔÉò Assistive Devices ÔÉò Functional Training ÔÉò Education and Home Exercise Program








