SJIA- SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS.pptx
- 1. SJIA- SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS BY: Dr. shekhar yadav Doctor of pharmacy
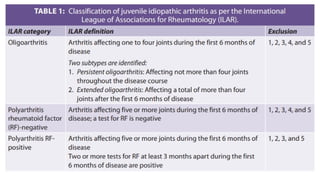
- 2. ŌĆó Chronic immune-mediated arthritis is previously known as juvenile chronic arthritis or juvenile rheumatoid arthritis. Currently, it is called juvenile idiopathic arthritis (JIA). The exact incidence and prevalence of JIA is unknown and likely varies across the world. ŌĆó According to the International League of Associations for Rheumatology (ILAR) criteria, JIA is defined as chronic arthritis (┬▒6 weeks duration) with no known cause occurring in children before the 16th birthday. ŌĆó The ILAR classification categorizes JIA into seven mutually exclusive categories based on the number of joints involved, extra-articular features, and serology identified in the first 6 months of disease presentation
- 6. ŌĆó About 10% to 20% of children with JIA have a rare and serious subtype called systemic juvenile idiopathic arthritis (SJIA). ŌĆó ŌĆ£SystemicŌĆØ means it may affect not only the joints but other parts of the body, including the liver, lungs and heart. ŌĆó SJIA, sometimes referred to as StillŌĆÖs disease, can occur any time during childhood, but it most commonly starts at about two years of age. Boys and girls are equally affected. ŌĆó SJIA also differs from other subtypes in that itŌĆÖs the only one considered an autoinflammatory rather than autoimmune disease. ŌĆó SJIA is more severe and can be more challenging to diagnose and treat than other types of juvenile idiopathic arthritis.
- 7. CAUSES ŌĆó Exactly what causes SJIA isn't clear. The general theory is that a child has a genetic predisposition, and the disease onset is triggered by something in the environment. The word ŌĆ£idiopathicŌĆØ means the cause or trigger is not known. Questions remain, but researchers are learning more about SJIA and why itŌĆÖs different from other types of juvenile arthritis. ŌĆó The body has two types of immunity ŌĆö innate and adaptive. The innate immune system is active at birth and is the first line of defense against infection. The adaptive immune system develops throughout life. Its role is to target and help to destroy viruses and bacteria that slip past the innate immune system.
- 8. ŌĆó Most forms of JIA develop when the adaptive immune system becomes overactive and attacks healthy cells and tissues. These disorders are called autoimmune diseases. Research suggests that SJIA is different. It may be an autoinflammatory condition that causes the innate immune system to be activated even when there is no infection to fight. Several factors have led researchers to think that SJIA is an autoinflammatory disease. For one thing, children with SJIA usually don't have autoantibodies in their blood, as many kids with other forms of JIA do. Autoantibodies are formed when the adaptive immune system is overactive. Also, kids with SJIA have high blood levels of two inflammatory proteins (cytokines) called interleukin-1 (IL-1) and interleukin-6 (IL-6). These proteins are known to cause inflammation in other autoinflammatory diseases and are believed to trigger inflammation in SJIA.
- 10. Macrophage Activation Syndrome ŌĆóa massive inflammatory response that overwhelms the whole body ŌĆóKnown triggers include viral infections, medication changes and flares ŌĆö a spike in disease activity. ŌĆóestimated 80% of cases are associated with SJIA
- 11. Lung and Heart Problems ŌĆó Doctors have seen more cases of lung diseases, such as pulmonary artery hypertension and interstitial lung disease, in children with SJIA. ŌĆó Pulmonary artery hypertension is high blood pressure that affects the arteries in the lungs and the right side of the heart. ŌĆó In interstitial lung disease, lung tissue becomes scarred, making it harder to get oxygen into the bloodstream. ŌĆó Parents should be alert for any signs of breathing problems, especially shortness of breath, and notify their pediatric rheumatologist as soon as possible.
- 12. Bones and Joints ŌĆó Persistent inflammation can slowly damage the joints, leading to reduced range of motion, loss of function, and sometimes the need for joint replacement early in life. ŌĆó SJIA, if not well controlled, is more likely than other types of juvenile arthritis to affect the jaw joint (the temporomandibular joint or TMJ), leading to a smaller-than- normal chin and changed appearance in some children. ŌĆó Fusion of the cervical spine (neck area) may also occur in kids with long-standing SJIA.
- 13. High blood pressure (hypertension) ŌĆó Hypertension can occur for at least two reasons. One is atherosclerosis ŌĆö the buildup of fatty deposits on artery walls. When the arteries narrow, the heart must pump harder to move blood through them. ŌĆó Although atherosclerosis can develop in healthy children, itŌĆÖs seen more often in SJIA ŌĆö likely due to ongoing inflammation. ŌĆó A more frequent cause of high blood pressure is treatment with corticosteroids, which cause fluid retention and weight gain.
- 14. SYMPTOMS
- 15. FEVER ŌĆó A high, recurring fever, often with a rash, is one of the first signs of SJIA. ŌĆó The fever usually follows a pattern in which a childŌĆÖs temperature reaches 103 degrees or higher, generally in the evening, and then drops within a few hours. ŌĆó Although a daily, spiking fever, typically in the evening, is one of the criteria for diagnosing SJIA, studies have shown that the pattern can vary. ŌĆó Sometimes the fever occurs in the morning or twice a day; occasionally, it may continue throughout the day.
- 16. RASH ŌĆóA flat, pale or pink rash, depending on the child's skin color, often appears on the childŌĆÖs trunk, arms or legs, although it can move from one part of the body to other parts. ŌĆó The rash may be itchy, but usually isnŌĆÖt. It tends to last a few minutes to a few hours and is associated with fever spikes.
- 17. JOINT PAIN ŌĆó The symptoms of joint swelling, pain, stiffness and warmth that occur are worse in the morning and after a nap or prolonged stillness. ŌĆó especially very young ones, often donŌĆÖt complain of joint pain with SJIA, but parents usually notice the onset of arthritis when a child starts to limp, seems stiff in the morning or suddenly becomes less active. ŌĆó Sometimes a single joint is affected, but more often several joints are involved, commonly the knees, wrists and ankles. Children with SJIA can also develop arthritis in the spine (in the neck area), jaw and hip joint.
- 18. ŌĆóSJIA symptoms may also come and go. Periods of lots of inflammation and worsening symptoms are called flares. A flare can last for days or months.
- 19. DIAGNOSIS
- 20. ŌĆó a diagnosis of SJIA requires ’ü▒a high fever for at least two weeks ’ü▒arthritis (joint pain and inflammation) in one or more joints for at least six weeks.
- 21. TESTING FOR SJIA
- 22. Health History ŌĆóTake a medical history to learn about past illnesses and current medications as well as details of current symptoms, such as how long a child has had them. ŌĆóKnowing the length of time that SJIA symptoms have been present helps rule out infections and other problems that can affect the joints temporarily.
- 23. Physical Exam ŌĆó Look for tenderness, warmth, swelling and reduced range of motion, especially in the knees, wrists, ankles and hip joints ŌĆö the ones most often affected by SJIA ŌĆö as well as in the jaw and neck. ŌĆójoint inflammation affects the growth centers in bones, causing them to be shorter than normal and possibly uneven from one side to another, so doctors assess limb length and overall growth.
- 24. Imagining tests ŌĆó X-ray (radiography) ŌĆó Computerized axial tomography (CAT or CT) scan ŌĆó Magnetic resonance imaging (MRI) ŌĆó Dual energy X-ray absorptiometry (DEXA or DXA) ŌĆó Discogram ŌĆó Video Fluoroscopy ŌĆó Arthrography ŌĆó Lower Body Nerve Evaluation ŌĆó Muscle Strength Evaluation ŌĆó Sciatic nerve stretch test ŌĆó Nerve Conduction Studies
- 26. Although SJIA canŌĆÖt be diagnosed with blood tests, certain laboratory findings can help support or disprove the diagnosis. ItŌĆÖs common for kids with SJIA to have the following: ŌĆó Extremely high white blood cell and platelet counts. ŌĆó Severe anemia due to poor iron absorption. ŌĆó Extremely high levels of ferritin, an iron-storing protein. ŌĆó Elevated inflammation markers, including erythrocyte sedimentation (sed) rate and C-reactive protein. ŌĆó No sign of antinuclear antibodies or rheumatoid factor antibodies ŌĆö both of which are often seen in the polyarticular form of juvenile idiopathic arthritis and other rheumatic diseases but rarely in SJIA.
- 28. TREATMENT
- 32. THALIDOMIDE IN SJIA PATIENTS Class of drug ŌĆō Angiogenesis Inhibitors And Antineoplastics Dose - 3 - 5 mg/kg/day MOA- It is a immunomodulator agent with an anti-angiogenesis effect in addition to inhibition of TNF- ╬▒, it also suppress other proinflammatory cytokines including IL-6. Efficacy is assessed by using juvenile arthritis disease activity score (JADAS) at 12th and 24th weeks of treatment. Adverse effects - sedation, somnolence, myalgia, constipation, neutropenia and anaphylaxis. peripheral neuropathy with long term use was also observed.
- 34. Non-Drug Therapies ŌĆó Although medication is the mainstay of SJIA treatment, but a regular exercise program is an also a important part of therapy. Exercise helps to build muscle strength, increase energy, and reduce pain and also helps maintain joint function and flexibility. ŌĆó Kids can participate in physical activities and team sports when their symptoms are well controlled, but they may have to limit certain activities during disease flares. ŌĆó A rehabilitation or physical therapist will likely be part of a child's treatment and can recommend the best activities.
- 36. THANK YOU