1 of 21
Downloaded 15 times



















Recommended
25. CTS due to median compression at the wrist



25. CTS due to median compression at the wristErik StĂĄlberg
Ěý
This document discusses median mononeuropathy at the wrist (MMW), also known as carpal tunnel syndrome (CTS). It describes the electrodiagnostic tests used to diagnose CTS, including motor and sensory nerve conduction studies of the median nerve across the carpal tunnel. Specific tests discussed include comparing median and ulnar sensory nerve action potentials from the digits to the wrist, and comparing median nerve latencies across the carpal tunnel versus from wrist to palm. The document provides reference values for different tests and degrees of abnormality defined by increased latencies and reduced amplitudes. It also discusses how local temperature can affect nerve conduction study results.4. Practical aspects



4. Practical aspectsErik StĂĄlberg
Ěý
Neurography is often the first test performed to evaluate peripheral nerve function. It focuses on answering the clinical question and follows strict methodological standards. The second step is typically EMG to further assess muscle and nerve function. Successive diagnostic steps depend on the findings and may include repetitive nerve stimulation, SFEMG, and macro EMG. Precise technique and attention to signal quality are important for optimally performing and interpreting neurography and EMG studies.AIDPCIDP MMN StĂĄlberg



AIDPCIDP MMN StĂĄlbergErik StĂĄlberg
Ěý
This document summarizes key information about Guillain-Barré syndrome (GBS) and related acute inflammatory neuropathies. It describes the incidence and subtypes of GBS, including typical symptoms such as weakness and sensory disturbances. Electrodiagnostic findings are outlined, including conduction block, prolonged distal latencies, and reduced nerve conduction velocities supportive of demyelination. The time course of GBS and potential etiologies like infection are mentioned. Chronic inflammatory demyelinating polyneuropathy (CIDP) and multifocal motor neuropathy are also summarized, with details on clinical features and electrodiagnostic patterns that help differentiate these conditions from GBS.CNE Jitter method



CNE Jitter methodErik StĂĄlberg
Ěý
1) The document provides guidelines for recording jitter with a concentric needle electrode (CNE), including definitions of acceptable CNE signals, techniques for voluntary and electrical stimulation activation, and potential errors in jitter measurements.
2) Examples are given of CNE recordings from different muscles that demonstrate normal voluntary activation, effects of varying stimulation frequency, axon reflex responses, and individual fiber blocking that is analyzed to determine jitter values.
3) Reference data from a multicenter study establishes normal mean jitter and maximum conduction delay (MCD) limits for different muscles based on CNE recordings.TM



TMErik StĂĄlberg
Ěý
The document discusses the use of telemedicine and networks in a neurophysiology laboratory. It describes:
1) How the lab uses networks and servers to share information, store patient data, and allow remote access to testing and reporting systems.
2) Examples of regional and international telemedicine collaborations, including video conferencing for consultations, remote supervision of testing, and quality assurance.
3) The future potential for telemedicine to develop national services, use smaller portable equipment, enable home monitoring, and facilitate international collaboration between individuals and research groups.32b. Conc Jitter



32b. Conc JitterErik StĂĄlberg
Ěý
This document discusses different types of EMG electrodes used to measure jitter, including concentric needle electrodes and single fiber EMG electrodes. It presents data from studies measuring jitter with these electrodes in various muscles. Specifically, it shows jitter measurements are higher with concentric needle electrodes than single fiber electrodes in muscles from myasthenia gravis patients. The document also reviews the sensitivity of different diagnostic tests for myasthenia gravis, with jitter analysis and repetitive nerve stimulation having high sensitivity to detect the condition.3. The MU Basics



3. The MU BasicsErik StĂĄlberg
Ěý
The motor unit consists of an anterior horn cell, nerve, neuromuscular junction, muscle fibers, and muscle unit. There are different types of muscle fibers (I, IIA, IIB/IIX, IIC) that vary in speed, fatigue resistance, and other properties. A normal motor unit contains 20-500 muscle fibers innervated by a single motor neuron. Electrophysiological techniques can study the structure and function of the motor unit, including reflexes, firing patterns, conduction studies, and EMG methods to assess motor unit number and characteristics.11. Myopati



11. MyopatiErik StĂĄlberg
Ěý
This document discusses electromyography (EMG) techniques for evaluating myopathies. It describes how EMG can detect spontaneous muscle fiber activity like fibrillation potentials, myotonic discharges, and complex repetitive discharges that indicate a myopathy. It also discusses EMG analysis of motor unit potential amplitudes and frequencies, interference patterns, and muscle fiber characteristics like splitting that provide clues about normal and diseased muscle. While EMG is sensitive in detecting many myopathies, it is not always specific for differentiating between specific muscle disease subtypes. EMG combined with other clinical findings can help classify myopathies and distinguish myopathic from neuropathic processes.19. Neurography principles



19. Neurography principlesErik StĂĄlberg
Ěý
This document provides an introduction and overview of neurography. It discusses the usefulness of neurography in evaluating polyneuropathies and local neuropathies. It describes different neurography methods and the physiological and anatomical functions assessed by motor neurography. The document outlines key parameters that are important for neurography from both technical and biological perspectives. It provides examples and discusses neurography of various peripheral nerves and the findings in different neuropathies.Decrement 171026



Decrement 171026Erik StĂĄlberg
Ěý
This document discusses testing for myasthenic disorders through repetitive nerve stimulation (RNS). It provides the RNS protocol of stimulating at 3Hz with 10 stimuli at rest, after 10 seconds of activity, and after 1 minute. Parameters like initial amplitude, decrement, and post-activity amplitude are analyzed. Several muscles are recommended for testing including deltoid, trapezius, and anconeus. Normal confidence limits for decrement in different muscles are provided. Examples of RNS results are shown for normal subjects, severe MG, LEMS, and congenital myasthenia. Potential pitfalls of RNS are also discussed.20. Late resp F H



20. Late resp F HErik StĂĄlberg
Ěý
This document discusses various late responses and reflexes that can be measured using electrophysiological testing, including F-waves, A-waves, H-reflexes, and flexion reflexes. It provides information on the generator site, mechanism, and normal values for many of these late responses. Examples of abnormal late responses are shown in various neurological conditions like diabetic neuropathy, radiculopathy, amyotrophic lateral sclerosis, and myasthenia gravis. The document aims to characterize the typical electrophysiological features of late responses and reflexes.ALS m Polio MMN



ALS m Polio MMNErik StĂĄlberg
Ěý
1) Neurophysiological tests play an important role in diagnosing and monitoring motor neuron disease (MND) such as amyotrophic lateral sclerosis (ALS).
2) Electromyography (EMG) can detect lower motor neuron signs in both clinically affected and unaffected regions, helping to confirm diagnosis and exclude other conditions. It analyzes motor unit potential (MUP) parameters and presence of fibrillation potentials and fasciculation potentials.
3) Nerve conduction studies can exclude other neuropathies but often find only mild or no sensory involvement in ALS patients. Motor unit number estimation quantifies the loss of motor units over time in ALS.6. Basic and Gemg



6. Basic and GemgErik StĂĄlberg
Ěý
This document discusses quantitative electromyography (QEMG) and what can be assessed using EMG. It outlines various muscle fiber characteristics and motor unit organization that EMG can evaluate, including number of fibers, grouping, and transmission at the neuromuscular junction. Parameters that can be quantified from concentric and monopolar EMG signals are described, such as spontaneous activity, motor unit potential (MUP) shape, recruitment, and dynamic changes over time. Various MUP parameters that provide information on motor unit size and characteristics are also defined. The document compares these parameters in evaluating different muscle disorders like neuropathy, myopathy and provides examples of quantitative analyses.Macro EMG



Macro EMGErik StĂĄlberg
Ěý
This document discusses macro electromyography (EMG), a technique used to study motor unit potentials (MUPs). Macro EMG involves inserting a cannula electrode into a muscle to record the electrical activity from many motor units at once, producing a macro motor unit potential (Macro MUP). The document also mentions multiunit triggered averaging, which averages Macro MUP signals to analyze individual motor unit characteristics from the combined signal.33. SFEMG in diseases



33. SFEMG in diseasesErik StĂĄlberg
Ěý
This document discusses single fiber electromyography (SFEMG) in the context of myasthenia gravis (MG), reinnervation, and myopathy. It provides criteria for abnormal SFEMG studies and normal jitter values. It shows that SFEMG can detect abnormalities in neuromuscular transmission in MG and other diseases. SFEMG is more sensitive than repetitive nerve stimulation and useful for diagnosing MG and investigating muscle membrane parameters, neuromuscular transmission, axonal conduction, and other factors.History SFEMG



History SFEMGErik StĂĄlberg
Ěý
This document discusses the development of single fiber electromyography (SFEMG) over time. Some key findings from SFEMG research include:
- SFEMG suggested that motor unit fibers are organized randomly rather than in subgroups, challenging previous theories.
- Propagation velocity along muscle fibers was measured, showing it decreases with activity and fatigue.
- The jitter phenomenon at the neuromuscular junction was identified as the source of variability in muscle fiber activation times.
- Technical developments like improved electrodes, filters, triggers and delay lines allowed more accurate measurement and understanding of single muscle fiber properties and motor unit organization.
SFEMG provided new insights into normal and diseased muscle physiology and remainsSFEMG Signal Atlas - Extensive - Stimulated



SFEMG Signal Atlas - Extensive - StimulatedErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Extensive - StimulatedSFEMG Signal Atlas - Highlights - Stimulated - Pitfalls - VRF - Axon Reflex



SFEMG Signal Atlas - Highlights - Stimulated - Pitfalls - VRF - Axon ReflexErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - Pitfalls - VRF - Axon ReflexSFEMG Signal Atlas - Extensive - Voluntary



SFEMG Signal Atlas - Extensive - VoluntaryErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Extensive - VoluntarySFEMG Signal Atlas - Highlights - Stimulated - Good Signals, Method



SFEMG Signal Atlas - Highlights - Stimulated - Good Signals, MethodErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - Good Signals, MethodSFEMG Signal Atlas - Highlights - Stimulated - FWaves, Extra Discharges



SFEMG Signal Atlas - Highlights - Stimulated - FWaves, Extra DischargesErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - FWaves, Extra DischargesSFEMG Signal Atlas - Highlights - Voluntary - Trig



SFEMG Signal Atlas - Highlights - Voluntary - TrigErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Voluntary - TrigSFEMG Signal Atlas - Highlights - Stimulated - Bad Signals



SFEMG Signal Atlas - Highlights - Stimulated - Bad SignalsErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - Bad SignalsSingle Fiber EMG (SFEMG) Signal Atlas - Introduction



Single Fiber EMG (SFEMG) Signal Atlas - IntroductionErik StĂĄlberg
Ěý
Single Fiber EMG (SFEMG) Signal Atlas - IntroductionSFEMG Signal Atlas - Highlights - Voluntary - Bad Signals



SFEMG Signal Atlas - Highlights - Voluntary - Bad SignalsErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Voluntary - Bad SignalsSFEMG Signal Atlas - Highlights - Voluntary - Good Signals, Method



SFEMG Signal Atlas - Highlights - Voluntary - Good Signals, MethodErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Voluntary - Good Signals, MethodQUIZ RNS



QUIZ RNSErik StĂĄlberg
Ěý
The patient has clinical features consistent with myasthenia gravis including fatigable neck and leg muscles as well as symptoms affecting swallowing and voice. Repetitive nerve stimulation and SFEMG testing would help confirm the diagnosis. Positive voltage-gated calcium channel antibodies also support MG. The diagnosis is myasthenia gravis (option a).QUIZ SFEMG



QUIZ SFEMGErik StĂĄlberg
Ěý
- To detect neurogenic blocking on SFEMG, you need to record 3 spikes simultaneously.
- To detect neurogenic jitter on SFEMG, you need to record 4 spikes simultaneously. If only 3 spikes are recorded, the jitter may be due to triggering issues rather than a neurogenic cause.
- To ascertain that distal and proximal stimulation is of the exact same axon during conduction velocity testing, stimulate distally and proximally simultaneously. If the proximal response disappears with dual stimulation, it indicates collision and the same axon was stimulated.NCS special



NCS specialErik StĂĄlberg
Ěý
The document contains questions and answers regarding neurophysiology techniques. Some key points discussed include:
- Voluntary activity does not influence CMAP amplitude at supramaximal stimulation, except for effects of muscle shortening.
- CMAP satellites can be distinguished from extra discharges by superimposing traces after 3Hz stimulation - satellites will be stable while extra discharges will be variable.
- If CMAP amplitude is unexpectedly low with no nerve damage or PNP, steps should be taken to check stimulation strength, equipment, skin conditions, and perform activation maneuvers before considering anomalies.
- F waves are usually normal in C8 radiculopathy but may be abnormal on the affected side in an ulNCS routine



NCS routineErik StĂĄlberg
Ěý
The document provides guidance on interpreting various neurography results. It discusses potential reasons for low amplitude compound muscle action potentials including carpal tunnel syndrome, lumbar epidural mass, technical problems, and polyneuropathy. It also discusses diagnoses for other neurography findings including possible carpal tunnel syndrome based on abnormal sensory findings in fingers 1-3 with normal motor amplitudes. Other sections discuss distinguishing between lumbar root lesions versus plexopathies and evaluating possible myasthenia gravis. The document aims to instruct on drawing conclusions from neurography studies.More Related Content
Viewers also liked (8)
19. Neurography principles



19. Neurography principlesErik StĂĄlberg
Ěý
This document provides an introduction and overview of neurography. It discusses the usefulness of neurography in evaluating polyneuropathies and local neuropathies. It describes different neurography methods and the physiological and anatomical functions assessed by motor neurography. The document outlines key parameters that are important for neurography from both technical and biological perspectives. It provides examples and discusses neurography of various peripheral nerves and the findings in different neuropathies.Decrement 171026



Decrement 171026Erik StĂĄlberg
Ěý
This document discusses testing for myasthenic disorders through repetitive nerve stimulation (RNS). It provides the RNS protocol of stimulating at 3Hz with 10 stimuli at rest, after 10 seconds of activity, and after 1 minute. Parameters like initial amplitude, decrement, and post-activity amplitude are analyzed. Several muscles are recommended for testing including deltoid, trapezius, and anconeus. Normal confidence limits for decrement in different muscles are provided. Examples of RNS results are shown for normal subjects, severe MG, LEMS, and congenital myasthenia. Potential pitfalls of RNS are also discussed.20. Late resp F H



20. Late resp F HErik StĂĄlberg
Ěý
This document discusses various late responses and reflexes that can be measured using electrophysiological testing, including F-waves, A-waves, H-reflexes, and flexion reflexes. It provides information on the generator site, mechanism, and normal values for many of these late responses. Examples of abnormal late responses are shown in various neurological conditions like diabetic neuropathy, radiculopathy, amyotrophic lateral sclerosis, and myasthenia gravis. The document aims to characterize the typical electrophysiological features of late responses and reflexes.ALS m Polio MMN



ALS m Polio MMNErik StĂĄlberg
Ěý
1) Neurophysiological tests play an important role in diagnosing and monitoring motor neuron disease (MND) such as amyotrophic lateral sclerosis (ALS).
2) Electromyography (EMG) can detect lower motor neuron signs in both clinically affected and unaffected regions, helping to confirm diagnosis and exclude other conditions. It analyzes motor unit potential (MUP) parameters and presence of fibrillation potentials and fasciculation potentials.
3) Nerve conduction studies can exclude other neuropathies but often find only mild or no sensory involvement in ALS patients. Motor unit number estimation quantifies the loss of motor units over time in ALS.6. Basic and Gemg



6. Basic and GemgErik StĂĄlberg
Ěý
This document discusses quantitative electromyography (QEMG) and what can be assessed using EMG. It outlines various muscle fiber characteristics and motor unit organization that EMG can evaluate, including number of fibers, grouping, and transmission at the neuromuscular junction. Parameters that can be quantified from concentric and monopolar EMG signals are described, such as spontaneous activity, motor unit potential (MUP) shape, recruitment, and dynamic changes over time. Various MUP parameters that provide information on motor unit size and characteristics are also defined. The document compares these parameters in evaluating different muscle disorders like neuropathy, myopathy and provides examples of quantitative analyses.Macro EMG



Macro EMGErik StĂĄlberg
Ěý
This document discusses macro electromyography (EMG), a technique used to study motor unit potentials (MUPs). Macro EMG involves inserting a cannula electrode into a muscle to record the electrical activity from many motor units at once, producing a macro motor unit potential (Macro MUP). The document also mentions multiunit triggered averaging, which averages Macro MUP signals to analyze individual motor unit characteristics from the combined signal.33. SFEMG in diseases



33. SFEMG in diseasesErik StĂĄlberg
Ěý
This document discusses single fiber electromyography (SFEMG) in the context of myasthenia gravis (MG), reinnervation, and myopathy. It provides criteria for abnormal SFEMG studies and normal jitter values. It shows that SFEMG can detect abnormalities in neuromuscular transmission in MG and other diseases. SFEMG is more sensitive than repetitive nerve stimulation and useful for diagnosing MG and investigating muscle membrane parameters, neuromuscular transmission, axonal conduction, and other factors.History SFEMG



History SFEMGErik StĂĄlberg
Ěý
This document discusses the development of single fiber electromyography (SFEMG) over time. Some key findings from SFEMG research include:
- SFEMG suggested that motor unit fibers are organized randomly rather than in subgroups, challenging previous theories.
- Propagation velocity along muscle fibers was measured, showing it decreases with activity and fatigue.
- The jitter phenomenon at the neuromuscular junction was identified as the source of variability in muscle fiber activation times.
- Technical developments like improved electrodes, filters, triggers and delay lines allowed more accurate measurement and understanding of single muscle fiber properties and motor unit organization.
SFEMG provided new insights into normal and diseased muscle physiology and remainsMore from Erik StĂĄlberg (18)
SFEMG Signal Atlas - Extensive - Stimulated



SFEMG Signal Atlas - Extensive - StimulatedErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Extensive - StimulatedSFEMG Signal Atlas - Highlights - Stimulated - Pitfalls - VRF - Axon Reflex



SFEMG Signal Atlas - Highlights - Stimulated - Pitfalls - VRF - Axon ReflexErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - Pitfalls - VRF - Axon ReflexSFEMG Signal Atlas - Extensive - Voluntary



SFEMG Signal Atlas - Extensive - VoluntaryErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Extensive - VoluntarySFEMG Signal Atlas - Highlights - Stimulated - Good Signals, Method



SFEMG Signal Atlas - Highlights - Stimulated - Good Signals, MethodErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - Good Signals, MethodSFEMG Signal Atlas - Highlights - Stimulated - FWaves, Extra Discharges



SFEMG Signal Atlas - Highlights - Stimulated - FWaves, Extra DischargesErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - FWaves, Extra DischargesSFEMG Signal Atlas - Highlights - Voluntary - Trig



SFEMG Signal Atlas - Highlights - Voluntary - TrigErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Voluntary - TrigSFEMG Signal Atlas - Highlights - Stimulated - Bad Signals



SFEMG Signal Atlas - Highlights - Stimulated - Bad SignalsErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Stimulated - Bad SignalsSingle Fiber EMG (SFEMG) Signal Atlas - Introduction



Single Fiber EMG (SFEMG) Signal Atlas - IntroductionErik StĂĄlberg
Ěý
Single Fiber EMG (SFEMG) Signal Atlas - IntroductionSFEMG Signal Atlas - Highlights - Voluntary - Bad Signals



SFEMG Signal Atlas - Highlights - Voluntary - Bad SignalsErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Voluntary - Bad SignalsSFEMG Signal Atlas - Highlights - Voluntary - Good Signals, Method



SFEMG Signal Atlas - Highlights - Voluntary - Good Signals, MethodErik StĂĄlberg
Ěý
SFEMG Signal Atlas - Highlights - Voluntary - Good Signals, MethodQUIZ RNS



QUIZ RNSErik StĂĄlberg
Ěý
The patient has clinical features consistent with myasthenia gravis including fatigable neck and leg muscles as well as symptoms affecting swallowing and voice. Repetitive nerve stimulation and SFEMG testing would help confirm the diagnosis. Positive voltage-gated calcium channel antibodies also support MG. The diagnosis is myasthenia gravis (option a).QUIZ SFEMG



QUIZ SFEMGErik StĂĄlberg
Ěý
- To detect neurogenic blocking on SFEMG, you need to record 3 spikes simultaneously.
- To detect neurogenic jitter on SFEMG, you need to record 4 spikes simultaneously. If only 3 spikes are recorded, the jitter may be due to triggering issues rather than a neurogenic cause.
- To ascertain that distal and proximal stimulation is of the exact same axon during conduction velocity testing, stimulate distally and proximally simultaneously. If the proximal response disappears with dual stimulation, it indicates collision and the same axon was stimulated.NCS special



NCS specialErik StĂĄlberg
Ěý
The document contains questions and answers regarding neurophysiology techniques. Some key points discussed include:
- Voluntary activity does not influence CMAP amplitude at supramaximal stimulation, except for effects of muscle shortening.
- CMAP satellites can be distinguished from extra discharges by superimposing traces after 3Hz stimulation - satellites will be stable while extra discharges will be variable.
- If CMAP amplitude is unexpectedly low with no nerve damage or PNP, steps should be taken to check stimulation strength, equipment, skin conditions, and perform activation maneuvers before considering anomalies.
- F waves are usually normal in C8 radiculopathy but may be abnormal on the affected side in an ulNCS routine



NCS routineErik StĂĄlberg
Ěý
The document provides guidance on interpreting various neurography results. It discusses potential reasons for low amplitude compound muscle action potentials including carpal tunnel syndrome, lumbar epidural mass, technical problems, and polyneuropathy. It also discusses diagnoses for other neurography findings including possible carpal tunnel syndrome based on abnormal sensory findings in fingers 1-3 with normal motor amplitudes. Other sections discuss distinguishing between lumbar root lesions versus plexopathies and evaluating possible myasthenia gravis. The document aims to instruct on drawing conclusions from neurography studies.EMG special



EMG specialErik StĂĄlberg
Ěý
A 21-year-old man presented with slowly progressive proximal muscle weakness and pain over 1 month. Neurography was normal. EMG showed myopathic motor unit potentials, interference patterns, and fibrillations. Ultrasound revealed hyperechogenicity and increased vascularization in the deltoid muscle. A muscle biopsy showed fiber diameter variation but no grouping. The likely diagnosis is polymyositis or dermatomyositis given the clinical presentation, normal neurography, myopathic EMG, and muscle biopsy findings.EMG routine



EMG routineErik StĂĄlberg
Ěý
The document discusses various EMG findings including: fibrillation potentials and positive sharp waves that are generated in the axon or individual muscle fibers with irregular firing rhythm and always signify axonal pathology; findings expected in demyelinating neuropathies with conduction block such as reduced MUP amplitudes and interference pattern; what complex repetitive discharges represent; and EMG findings in acute weakness such as Guillain-Barré syndrome where early on there would be normal CMAPs and CVs with reduced interference pattern. It also addresses discrepancies that can occur on EMG and the diagnostic methods of choice for various conditions.RNS



RNSErik StĂĄlberg
Ěý
This document discusses neuromuscular transmission testing, including repetitive nerve stimulation (RNS) protocols and analysis. It describes RNS protocols to evaluate myasthenia gravis and other neuromuscular disorders. Key points covered include RNS parameters to analyze like initial amplitude, decrement, and post-activation facilitation/exhaustion. It also discusses RNS considerations like muscle selection, temperature, and fixation effects. Normal RNS results and examples of abnormal findings in myasthenia gravis and congenital myasthenia are presented.EMG NCS Scoring



EMG NCS ScoringErik StĂĄlberg
Ěý
This document describes several classification systems for analyzing electromyography (EMG) results:
1. It classifies the degree of acute or subacute denervation seen on EMG as slight, moderate, or severe based on the duration of symptoms and EMG findings like fibrillation potentials and insertional activity.
2. It provides criteria for possible, probable, or definite myopathy based on spontaneous activity, motor unit potential morphology and instability, and involvement of muscle groups on EMG.
3. It outlines a quantitative EMG scoring system for evaluating myopathic changes with criteria in several categories.
4. It proposes a grading system for axonal and demyelinating peripheral neuropathy basedEDX Facialis
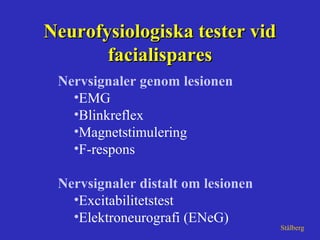
- 1. Neurofysiologiska tester vidNeurofysiologiska tester vid facialisparesfacialispares Nervsignaler genom lesionen •EMG •Blinkreflex •Magnetstimulering •F-respons Nervsignaler distalt om lesionen •Excitabilitetstest •Elektroneurografi (ENeG) Stålberg
- 2. Engström -98 reg stim Elektrodplacering vidElektrodplacering vid neurografi av facialisnervenneurografi av facialisnerven
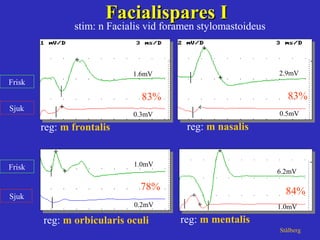
- 3. reg: m orbicularis oculi reg: m frontalis Sjuk Frisk Sjuk Frisk Facialispares IFacialispares I StĂĄlberg 1.6mV 0.3mV 83% 1.0mV 0.2mV 78% stim: n Facialis vid foramen stylomastoideus reg: m nasalis 2.9mV 0.5mV 83% 6.2mV 1.0mV 84% reg: m mentalis
- 4. Neurografi vid facialispares avNeurografi vid facialispares av lätt, måttlig och uttalad svårighetsgradlätt, måttlig och uttalad svårighetsgrad Days Ampl asym mean % Thomander-91
- 5. Days Thomander-91 Ampl asym range (I,III) % Neurografi vid facialis paresNeurografi vid facialis pares Skillnaden vid lätt och uttalad svårighetsgradSkillnaden vid lätt och uttalad svårighetsgrad 0 - - - - - - - - - - - 50 75 100 I III 1 2 3 4 5 10 20 50 100 200 500 1000 I I I I I I I I I I I I
- 6. Principer för läkning Neurapraxi Konduktionsblocket släpper funktion inom 1-3 veckor Axonal degeneration Partiell skada, distal nervutväxt funktion inom 3-6 mån Total skada, nyutväxt av axon function efter > 6mån Vid kombinerad patofysiologi alltså förbättring i 2 steg; jonkanaler, regeneration
- 7. Trigeminal nerve stim left side
- 8. BlinkreflexenBlinkreflexen n Trigeminus (V) och n Facialis (VII)n Trigeminus (V) och n Facialis (VII)
- 9. Normal blinkreflexNormal blinkreflex stim: n trigeminus supraorbitalis reg: m orbicularis oculi bilat StĂĄlberg
- 10. Patologisk blinkreflex paralys (sin)Patologisk blinkreflex paralys (sin) stim: n trigeminus supraorbitalis reg: m orbicularis oculi bilat StĂĄlberg sjuk sida
- 11. stim: n trigeminus supraorbitalis reg: m orbicularis oculi bilat Patologisk blinkreflex partiell pares (dx)Patologisk blinkreflex partiell pares (dx) StĂĄlberg sjuk sida
- 13. EMG vid facialisparesEMG vid facialispares beskriver: •Denervation = axonal degeneration •Reinnervation (pågående/avslutad) •Grad av aktivitetsförlust •Tecken på synkinesi •Tecken på kontralateral överinnervation Stålberg
- 14. Reinnervation i orb. oculi efterReinnervation i orb. oculi efter Facialispares, 3 mĂĄnFacialispares, 3 mĂĄn normalnormal reinnervationreinnervation StĂĄlberg
- 15. Andra frågeställningar för neurofysiologi i ansiktet 1. Är trigeminus intakt? 2. Nervgraftets funtion 3. Överinnervation från kontralaterala sidan
- 16. Ansiktstrauma för 5 mån sedan. Facialis u.a. men domningar ENeG normal
- 17. Trig stim sjuk sida; inget ipsi-eller contralateralt facialis-svar ( ) Stim frisk sida; normalt facialissvar från frisk och sjuk sida Inget facialissvar på grund av trig patologi Här finns facialissvar efter kontralateral trig stimulering sjuk sjuk frisk frisk
- 18. ENeG nervgraft Symmetrisk, normal Tydlig asymmetri, lĂĄgt svar pĂĄ sjuk sida dvs graftet har endast MĂĄttlig effekt
- 19. Innervation från frisk sida över meddellinjen några cm
- 20. Right sided posttraumatic facial palsy Some voluntary activity near the midline but no response on ipsilateral nerve stimulation Reinnervation from healthy side no activity no activity frisk sida sjuk sida
- 21. Konklusion • Preoperativ neurofysiologi ej relaterad till postoperativa komplikationer • Post-operativ neurofysiologi (ENeG, blinkreflex, EMG) ger prognostisk vägledning Edfeldt et al 2003