Hypertension according to latest clinical advances
- 1. ETIOPATHOGENESIS AND PHARMACOTHERAPY OF DISEASE ASSOCIATED WITH HYPERTENSION PRESENTED BY ARBEENA SHAKIR
- 2. 01 DEFINITION AND ITS CLASSIFICATION ETIOPATHOGENESIS OF HYPERTENSION TREATMENT OF HYPERTENSION RECENT CLINICAL ADVANCES COMPELLING INDICATION 04 02 05 03 Table of contents
- 4. DEFINITION OF HYPERTENSION Hypertension is progressive CV disorder arising from a complex and interrelated etiologies Hypertension is de’¼üned by presence of a chronic elevation of systemic arterial presssure above a certain threshold value of above 140/90 mmHg . Progression of hypertension is strongly associated with functional and structural cardiac and vascular abnormalities that damage the heart,kidneys,brain,vasculature,and other organs and leads to premature morbidity and death.
- 5. Stages of hypertension according to AHA
- 7. Etiopathogenesis of hypertension ŌĆö--Diagram representing the renin-angiotensin-aldostrerone systemŌĆö----
- 8. 1. Arterial sti’¼Ćness Arterial stiffness refers to a reduction in elasticity and distensibility of arteries, and pulse wave velocity (PWV) is often used to represent the degree of stiffness in large arteries. An increase in PWV indicates severe arterial stiffness and impaired in arterial dilatation capacity. systolic BP is also associated with a clinically signi’¼ücant progression of arterial stiffness . It is still a ŌĆ£chicken and egg questionŌĆØ that elevated blood pressure and arterial stiffness which come ’¼ürst. Water-sodium retention is a key cause of abnormal increases in intravascular fluid volume. Diuretics (especially thiazide diuretics) are important in the control of hypertension caused by water-sodium retention. Except secondary hypertension resulted from renal dysfunction, there is also a group of hypertensive patients related to water-sodium retention in essential hypertension, namely salt-sensitive hypertension. Reducing sodium intake has been considered as an important way to reduce the incidence of hypertension. However, the bene’¼üts of using salt with low doses of sodium remain controversial, since low sodium intake is also associated with an increased risk of cardiovascular disease. 2. Water-sodium retention and salt sensitive
- 9. Renin-angiotensin-aldosterone system is a consecutive peptidergic system that functions in the control of the renal, adrenal, and cardiovascular systems. RAAS regulates BP mainly by affecting arterial constriction and water-sodium retention in the body. Both circulating RAAS and tissue RAAS (cardiac RAAS, vascular RAAS, intra-renal RAAS, brain RAAS and adipose tissue RAAS) have been involved in the pathogenesis of essential hypertension and related target organ damage. 3. Renin-angiotensin-aldosterone system Several components of axis cascade have been identi’¼üed in the RAAS, including angiotensinogen, renin, angiotensin-converting enzyme, angiotensins with various subtypes (Ang I, Ang II, Ang III, Ang IV, Ang 1-7), aldosterone and aldosterone receptors. Among these, angiotensinogen, produced by the liver, is the starting point of the system. 4.Sympathetic dysregulation Sympathetic dysregulation is also an important cause of essential hypertension. The sympathetic overdrive leads to increased cardiac output, increased systemic vascular tone, and elevated plasma catecholamine levels. Patients with hypertension can manifest as greater muscle sympathetic nerve activity (MSNA) and lower baroreflex response .
- 10. 5. Genetics Hypertension is closely associated with genes, and our understanding of the relationship between genetics and BP has been well improved in recent years. More than 500 loci involved in the regulation of BP have been revealed by genome-wide association studies, taking the total number of BP genetic loci to over 1,000. Genetics alone is not suf’¼ücient to explain the variability in BP, suggesting that other risk factors are involved, such as epigenetic modi’¼ücations. Emerge evidence demonstrated potential contribution of epigenetic mechanisms in essential hypertension. INTERACTION BETWEEN THE PATHOGENESIS OF HYPERTENSION :
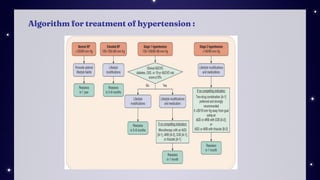
- 12. Goal of treatment : The overall goal is to reduce morbidity and mortality by the least intrusive means possible. JNC7 guidelines recommend goal BP less than 140/90 mmHg for most patients, less than 140/80 mm Hg for patients with diabetes mellitus, and less than 130/80 mm Hg for patients with CKD who have persistent albuminuria (>30 mg urine albumin excretion per 24 hours). Non-pharmacological therapy Lifestyle modi’¼ücations: (1) weight loss if overweight, (2) adoption of the Dietary Approaches to Stop Hypertension (DASH) eating plan, (3) dietary sodium restriction ideally to 1.5 g/day (3.8 g/day sodium chloride), (4) regular aerobic physical activity, (5) moderate alcohol consumption (two or fewer drinks per day), and (6)smoking cessation. ŌĆó Lifestyle modi’¼ücation alone is suf’¼ücient for most patients with prehypertension but inadequate for patients with hypertension and additional CV risk factors or hypertension-associated target-organ damage.
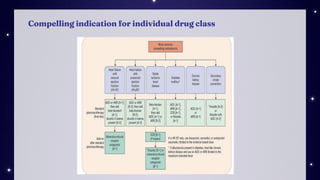
- 13. Pharmacological therapy Initial drug selection depends on the degree of BP elevation and presence of compelling indications for selected drugs. ŌĆó Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), calcium channel blockers (CCBs), and thiazide diuretics are acceptable ’¼ürst-line options. ŌĆó╬▓-Blockers are used to either treat a speci’¼üc compelling indication or as combination therapy with a ’¼ürst-line antihypertensive agent for patients without a compelling Indication. ŌĆó Most patients with stage 1 hypertension should be treated initially with a ’¼ürst-line antihypertensive drug or a two-drug combination. Combination therapy is recommended for patients with stage 2 hypertension, preferably with two ’¼ürst-line agents. ŌĆó There are six compelling indications where speci’¼üc antihypertensive drug classes provide unique bene’¼üts. ŌĆó Other antihypertensive drug classes (╬▒1-blockers, direct renin inhibitors, central ╬▒2 agonists, peripheral adrenergic antagonists, and direct arterial vasodilators) are alternatives that may be used for select patients after ’¼ürst-line agents .
- 14. First line and other common antihypertensive drug :
- 15. Algorithm for treatment of hypertension :
- 16. Compelling indication for individual drug class
- 18. The European Society of Cardiology and the European Society of Hypertension (ESC/ESH) de’¼üne hypertension by of’¼üce BP levels Ōēź140 mmHg systolic or 90 mmHg diastolic, the American Heart Association (AHA), the American College of Cardiology (ACC) and other scienti’¼üc societies have endorsed a more ŌĆśaggressiveŌĆÖ de’¼ünition based on of’¼üce BP values Ōēź130 mmHg systolic or 80 mmHg diastolic. In addition, the International Society of Hypertension (ISH) adopted the 140/90 mmHg de’¼ünition. Of note, the more aggressive diagnostic targets endorsed by the US guidelines do no imply that all subjects with of’¼üce BP in the range of 130ŌĆō139/80ŌĆō89 mmHg require drug treatment. Instead, the AHA/ACC guidelines suggest to apply more appropriate life-style measures (weight control, smoking cessation, low-sodium diet, etc.) for these subjects, and to reserve drug treatment for cases of inef’¼ücacy of non-pharmacologic measures.
- 19. 1.endothelin receptor antagonists Endothelin regulates vascular tone and BP, producing a powerful vasoconstrictor effect and contributing to the pathogenesis of hypertension. It causes neurohormonal and sympathetic activation, hypertensive end-organ damage, ’¼übrosis, endothelial dysfunction, and increased aldosterone synthesis and secretion. Furthermore, endothelin-1 (ET-1, the biologically predominant member of the endothelin peptide family) is an endothelial cell-derived peptide with a wide variety of developmental and physiological functions, which include embryogenesis and nociception.. More speci’¼ücally, the endothelin system plays a role in regulating the development of the speci’¼üc neural crest cell population and its derivatives
- 20. Aprocinentan, a blocker of both endothelin-A and endothelin-B receptors with a very long pharmacological half-life (about 44 h), proved more effective than placebo and lisinopril. Interestingly, this antihypertensive agent seems to exert additional mechanisms beyond the expected bene’¼ücial effects of sustained BP-lowering action (including a decrease in renal vascular resistance and left ventricular hypertrophy) supporting the hypothesis that this new agent could expand our antihypertensive arsenal in resistant hypertension. Indeed, aprocitentan in patients with resistant hypertension is currently under investigation in the PRECISION phase III trial. 2. Neprilysin Combined with Renin-Angiotensin System Inhibition Neprilysin, a zinc endopeptidase, inactivates, not only the cardiac natriuretic peptides, but also bradykinin,thereby inducing vasodilatation and natriuresis resulting from a more prolonged action by these agents]. Neprilysin was not developed as monotherapy for clinical use, but combined with drugs that inhibit the renin-angiotensin-aldosterone system.
- 21. 3. Angiotensin II Receptor Agonists Angiotensin II induces vasoconstriction by stimulating the angiotensin 1 receptors, and vasodilatation by stimulating the angiotensin 2 receptors. In experimental and clinical settings, stimulation of angiotensin 2 receptors inhibits ’¼übrosis and induces vasodilatation, natriuresis, and blood pressure reduction. Consequently, angiotensin II receptor agonists display an interesting antihypertensive potential and are currently investigated for ef’¼ücacy and safety. 4. Sodium-Glucose Cotrasporter-2 Inhibitors In pivotal phase III clinical trials, selective SGLT2 receptor inhibitors empagliflozin, canagliflozin, dapagliflozin and ertugliflozin modestly reduced systolic and diastolic BP through various mechanisms which may include natriuresis, osmotic diuresis and reduction of the sympathetic tone. These drugs induced a marked reduction in the risk of heart failure . In patients with heart failure and reduced ejection fraction (HFrEF), both with and without diabetes, empagliflozin and dapagliflozin reduced cardiovascular mortality and the need of re-hospitalizations for heart failure. In patients with heart failure with preserved ejection fraction (HFpEF), empagliflozin signi’¼ücantly reduced the risk of cardiovascular death or hospitalization for heart failure by 21%
- 22. In the EMPA-REG BP trial, empagliflozin 10 mg and 25 mg reduced 24-h ambulatory BP by 3.44/4.16 mmHg more than placebo and the degree of antihypertensive effect was comparable in the presence of none, one or more than one antihypertensive drug 5. Renal Denervation Renal sympathetic overactivity contributes to the development and progression of hypertension. Renal denervation in experimental models of hypertension has been shown to reduce BP and improve renal function, which laid the foundation for its introduction to clinical practice. Some clinical trials published over the past 15 years generated many expectations on the clinical utility of renal denervation.. Unfortunately, the SIMPLICITY HTN-3 trials failed to demonstrate the superiority of renal denervation over sham control in terms of BP lowering effect. However, the SIMPLICITY HTN-3 trials had several methodological shortcomings. Just to mention some of these limitations, the study erroneously included patients with secondary hypertension (hyperaldosteronism, etc.), 34% of operators had executed only one denervation procedure in the past, drug treatment was much more intense in the ŌĆśshamŌĆÖ control group than in the denervation group, denervation was not ŌĆścompleteŌĆÖ (not all quadrants of renal artery were ablated) in 75% of cases. Thus, the entire issue was reconsidered, with planning and execution of newer better-designed clinical trials, which provided positive results
- 23. The main e’¼Ćects of inhibition of a’¼Ćerent and e’¼Ćerent sympathetic activity induced by renal denervation.
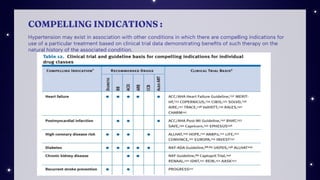
- 24. COMPELLING INDICATIONS : Hypertension may exist in association with other conditions in which there are compelling indications for use of a particular treatment based on clinical trial data demonstrating bene’¼üts of such therapy on the natural history of the associated condition.
- 25. 1. Ischemic Heart Disease pharmacologic therapy should be initiated with a BB.142,156 BBs will lower BP; reduce symptoms of angina; improve mortality; and reduce cardiac output, heart rate, and AV conduction. If angina and BP are not controlled by BB therapy alone, or if BBs are contraindicated, as in the presence of severe reactive airways disease, severe peripheral arterial disease, high-degree AV block, or the sick sinus syndrome, either long-acting dihydropyridine or nondihydropyridine type CCBs may be used. 2. Heart failure The inexorable progression to more severe stages of left ventricular dysfunction can be signi’¼ücantly reduced by effective therapy with ACEIs, BBs, and diuretics. Hypertension precedes the development of HF in approximately 90 percent of patients and increases risk for HF by two- to threefold. Hypertension is especially important in HF affecting African American and elderly persons. HF is a ŌĆ£compelling indicationŌĆØ for the use of ACEI. Abundant evidence exists to justify their use with all stages of HF (table 12). In patients intolerant of ACEIs, ARBs may be used. BBs are also recommended in HF because of clinical studies demonstrating decreased morbidity and mortality, and improvement in HF symptoms
- 26. 3. Diabetes and hypertension The concordance of hypertension and diabetes is increased in the population; hypertension is disproportionately higher in diabetics, while persons with elevated BP are two and a half times more likely to develop diabetes within 5 years. Regarding the selection of medications, clinical trials with diuretics, ACEIs, BBs, ARBs, and calcium antagonists have a demonstrated bene’¼üt in the treatment of hypertension in both type 1 and type 2 diabetics. 4. Chronic kidney disease The joint recommendations of the American Society of Nephrology and the National Kidney Foundation provide useful guidelines for management of hypertensive patients with CKD. They recommend a goal BP for all CKD patients of <130/80 mmHg and the need for more than one antihypertensive drug to achieve this goal. The guidelines indicate that most patients with CKD should receive an ACEI or an ARB in combination with a diuretic, and many will require a loop diuretic rather than a thiazide.
- 27. 5. Patients With Cerebrovascular Disease With respect to the prevention of recurrent stroke, PROGRESS demonstrated that addition of the diuretic, indapamide, to the ACEI, perindopril, caused a 43 percent reduction in stroke occurence.The reduced incidence of stroke appeared related to the BP reduction obtained by the combination therapy even though many patients on entry into the study were not hypertensive.No signi’¼ücant reduction was present in those on perindopril alone whose BP was only 5/3 mmHg lower than in the control group.
- 28. REFERENCES : ŌŚÅ Joseph T. Dipiro, pharmacotherapy : a pathophysiological approach, 11th edition chapter 30 pg-273-308 ŌŚÅ Joseph T. Dipiro, pharmacotherapy handbook ,9th edition chapter 10 pg-87-90 ŌŚÅ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8949859/#sec4-jcdd-09-00072title ŌŚÅ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9616110/ ŌŚÅ Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) (nih.gov)
















![Aprocinentan, a blocker of both endothelin-A and endothelin-B receptors with a very long pharmacological
half-life (about 44 h), proved more effective than placebo and lisinopril. Interestingly, this antihypertensive
agent seems to exert additional mechanisms beyond the expected bene’¼ücial effects of sustained BP-lowering
action (including a decrease in renal vascular resistance and left ventricular hypertrophy) supporting the
hypothesis that this new agent could expand our antihypertensive arsenal in resistant hypertension. Indeed,
aprocitentan in patients with resistant hypertension is currently under investigation in the PRECISION phase III
trial.
2. Neprilysin Combined with Renin-Angiotensin System Inhibition
Neprilysin, a zinc endopeptidase, inactivates, not only the cardiac natriuretic peptides, but also
bradykinin,thereby inducing vasodilatation and natriuresis resulting from a more prolonged action by
these agents]. Neprilysin was not developed as monotherapy for clinical use, but combined with drugs
that inhibit the renin-angiotensin-aldosterone system.](https://image.slidesharecdn.com/hypertension3-231009115259-7eab6197/85/Hypertension-according-to-latest-clinical-advances-20-320.jpg)