Ictus
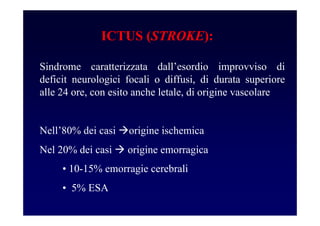
- 2. Sindrome caratterizzata dallŌĆÖesordio improvviso di deficit neurologici focali o diffusi, di durata superiore alle 24 ore, con esito anche letale, di origine vascolare NellŌĆÖ80% dei casi origine ischemica Nel 20% dei casi origine emorragica ICTUS (STROKE): ŌĆó 10-15% emorragie cerebrali ŌĆó 5% ESA
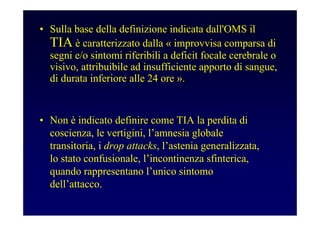
- 3. ŌĆó Sulla base della definizione indicata dall'OMS il TIA ├© caratterizzato dalla ┬½ improvvisa comparsa di segni e/o sintomi riferibili a deficit focale cerebrale o visivo, attribuibile ad insufficiente apporto di sangue, di durata inferiore alle 24 ore ┬╗. ŌĆó Non ├© indicato definire come TIA la perdita di coscienza, le vertigini, lŌĆÖamnesia globale transitoria, i drop attacks, lŌĆÖastenia generalizzata, lo stato confusionale, lŌĆÖincontinenza sfinterica, quando rappresentano lŌĆÖunico sintomo dellŌĆÖattacco.
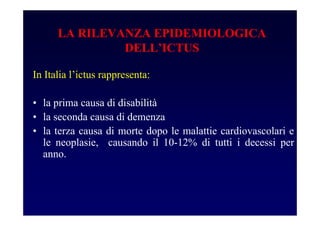
- 4. In Italia lŌĆÖictus rappresenta: ŌĆó la prima causa di disabilit├Ā ŌĆó la seconda causa di demenza ŌĆó la terza causa di morte dopo le malattie cardiovascolari e le neoplasie, causando il 10-12% di tutti i decessi per anno. LA RILEVANZA EPIDEMIOLOGICA DELLŌĆÖICTUS
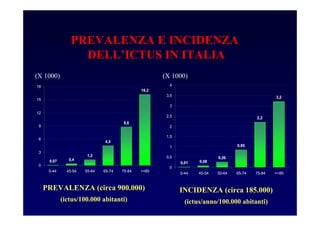
- 5. 16,2 8,8 0,4 1,3 4,5 0,07 0 3 6 9 12 15 18 0-44 45-54 55-64 65-74 75-84 >=85 0,01 0,08 0,26 0,85 2,2 3,2 0 0,5 1 1,5 2 2,5 3 3,5 4 0-44 45-54 55-64 65-74 75-84 >=85 PREVALENZA (circa 900.000) (ictus/100.000 abitanti) INCIDENZA (circa 185.000) (ictus/anno/100.000 abitanti) PREVALENZA E INCIDENZA DELLŌĆÖICTUS IN ITALIA (X 1000) (X 1000)
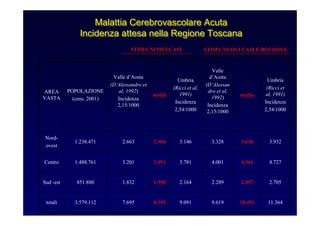
- 6. 11.36410.4919.6199.0918.3937.6953.579.112totali 2.7052.4972.2892.1641.9981.832851.880Sud -est 4.7274.3644.0013.7813.4913.2011.488.761Centro 3.9323.6303.3283.1462.9042.6631.238.471 Nord- ovest Umbria (Ricci et al, 1991) Incidenza 2,54/1000 media Valle dŌĆÖAosta (DŌĆÖAlessan dro et al, 1992) Incidenza 2,15/1000 Umbria (Ricci et al, 1991) Incidenza 2,54/1000 media Valle dŌĆÖAosta (DŌĆÖAlessandro et al, 1992) Incidenza 2,15/1000 POPOLAZIONE (cens. 2001) AREA VASTA STIMA NUOVI CASI STIMA NUOVI CASI E RECIDIVE Malattia Cerebrovascolare Acuta Incidenza attesa nella Regione Toscana Malattia Cerebrovascolare AcutaMalattia Cerebrovascolare Acuta Incidenza attesa nella Regione ToscanaIncidenza attesa nella Regione Toscana
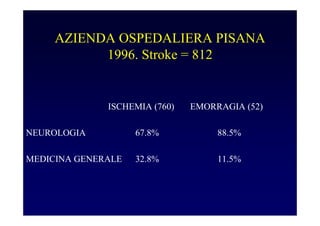
- 7. AZIENDA OSPEDALIERA PISANA 1996. Stroke = 812 ISCHEMIA (760) EMORRAGIA (52) NEUROLOGIA 67.8% 88.5% MEDICINA GENERALE 32.8% 11.5%
- 8. FATTORI DI RISCHIO NON MODIFICABILI Et├Ā (lŌĆÖincidenza di ictus aumenta con lŌĆÖet├Ā e dopo i 55 anni raddoppia per ogni decade) Sesso (lŌĆÖincidenza di ictus ├© maggiore nei maschi ma la differenza fra sessi si riduce con lŌĆÖet├Ā) Familiarit├Ā e razza ( il ruolo dei fattori genetici nella determinazione del rischio di ictus non ├© tuttora definito)
- 9. FATTORI DI RISCHIO MODIFICABILI BEN DOCUMENTATI ŌĆó Ipertensione arteriosa ŌĆó Alcune cardiopatie ŌĆó Diabete mellito ŌĆó Iperomocisteinemia ŌĆó Ipertrofia ventricolare sinistra ŌĆó Stenosi carotidea asintomatica ŌĆó Fumo di sigaretta ŌĆó Attacco ischemico transitorio (TIA) (Rischio ictus: 11.6% entro un anno, 5.9%/anno nei successivi 4 anni) Fibrillazione atriale Endocardite infettiva Stenosi mitralica Infarto miocardico esteso e recente
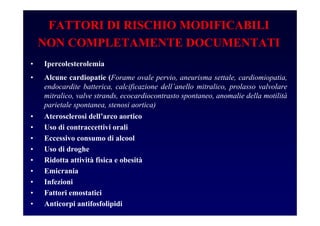
- 10. FATTORI DI RISCHIO MODIFICABILI NON COMPLETAMENTE DOCUMENTATI ŌĆó Ipercolesterolemia ŌĆó Alcune cardiopatie (Forame ovale pervio, aneurisma settale, cardiomiopatia, endocardite batterica, calcificazione dellŌĆÖanello mitralico, prolasso valvolare mitralico, valve strands, ecocardiocontrasto spontaneo, anomalie della motilit├Ā parietale spontanea, stenosi aortica) ŌĆó Aterosclerosi dellŌĆÖarco aortico ŌĆó Uso di contraccettivi orali ŌĆó Eccessivo consumo di alcool ŌĆó Uso di droghe ŌĆó Ridotta attivit├Ā fisica e obesit├Ā ŌĆó Emicrania ŌĆó Infezioni ŌĆó Fattori emostatici ŌĆó Anticorpi antifosfolipidi
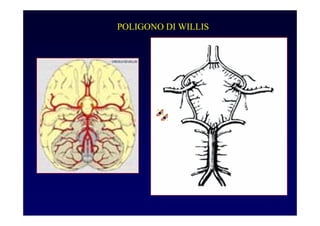
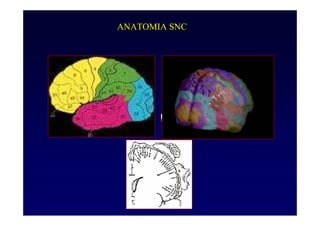
- 12. ANATOMIA SNC
- 13. CLASSIFICAZIONE SU BASE FISIOPATOLOGICA DEI SOTTOTIPI DELLŌĆÖICTUS ISCHEMICO CRITERI DEL Trial of ORG 10172 in AcuteStrokeTreatment (TOAST), 1993 1. Aterosclerosi dei vasi di grosso calibro 2. Cardioembolia(possibile/probabile) 3. Occlusione dei piccoli vasi 4. Ictus da cause diverse 5. Ictus da cause non determinate
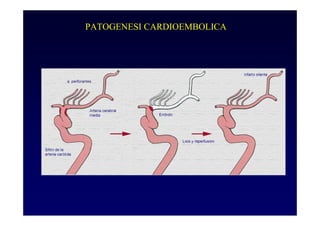
- 16. STROKE CARDIOEMBOLICO ŌĆó Fibrillazione atriale non valvolare ŌĆó IMA recente ŌĆó Protesi valvolare ŌĆó Stenosi mitralica reumatica ŌĆó Trombo ventricolo sin ŌĆó Mixoma atriale ŌĆó Endocardite infettiva ŌĆó Miocardiopatia dilatativa ŌĆó Forame ovale pervio (poss.) ŌĆó Stenosi calcifica dellŌĆÖaorta (poss.) ŌĆó Prolasso mitrale ŌĆó Calcificazione anulus mitralico
- 17. SINDROMI LACUNARI ŌĆóSTROKE MOTORIO PURO ŌĆóSTROKE SENSITIVO PURO ŌĆóEMIPARESI ATASSICA ŌĆóDISARTRIA CON ADIADOCOCINESIA DELLA MANO ŌĆóDISARTRIA PURA ŌĆóDEFICIT OCULOMOZIONE ŌĆóEMICOREA EMIBALLISMO ŌĆóDISTONIA FOCALE ŌĆóPARKINSONISMO (?) ŌĆóSTROKE SENSITIVO-MOTORIO
- 18. VASCULITI CEREBRALI vasculopatie infiammatorie primarie arterite a cellule giganti arterite di Takayasu Lupus eritematoso sistemico sindrome di Sneddon vasculiti necrotizzanti sistemiche poliarterite nodosa sindrome di Churg-Strauss granulomatosi di Wegener artrite reumatoide sindrome di Sj├Čgren malattia di Beh├¦et sclerodermia sarcoidosi arterite isolata del sistema nervoso centrale malattia di B├╝rger vasculopatie infiammatorie secondarie infezioni farmaci radiazioni morbo celiaco malattie infiammatorie intestinali
- 19. DISORDINI COAGULAZIONE E STROKE Riduzione dei livelli degli inibitori della coagulazione -Anti-trombinaIII -ProteinaC -ProteinaS -Co-fattoreII dellŌĆÖeparina Resistenza alla proteinaC attivata(aPCresistance) Aumento dei livelli dei fattori della coagulazione -Fibrinogeno -FattoreVII Condizioni dismetabolichepro-trombotiche -Iperomocisteinemia -Ipertrigliceridemia -IperLp(a)
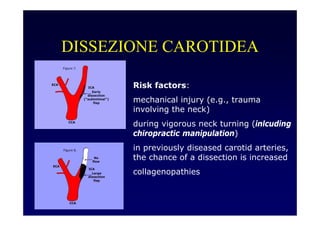
- 20. DISSEZIONE CAROTIDEA Risk factors: mechanical injury (e.g., trauma involving the neck) during vigorous neck turning (inlcuding chiropractic manipulation) in previously diseased carotid arteries, the chance of a dissection is increased collagenopathies
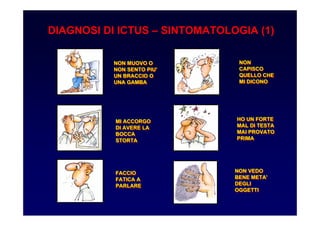
- 21. NON MUOVO O NON SENTO PIU' UN BRACCIO O UNA GAMBA NON MUOVO O NON SENTO PIU' UN BRACCIO O UNA GAMBA MI ACCORGO DI AVERE LA BOCCA STORTA MI ACCORGO DI AVERE LA BOCCA STORTA HO UN FORTE MAL DI TESTA MAI PROVATO PRIMA HO UN FORTE MAL DI TESTA MAI PROVATO PRIMA FACCIO FATICA A PARLARE FACCIO FATICA A PARLARE NON CAPISCO QUELLO CHE MI DICONO NON CAPISCO QUELLO CHE MI DICONO NON VEDO BENE META' DEGLI OGGETTI NON VEDO BENE META' DEGLI OGGETTI DIAGNOSI DI ICTUS ŌĆō SINTOMATOLOGIA (1)
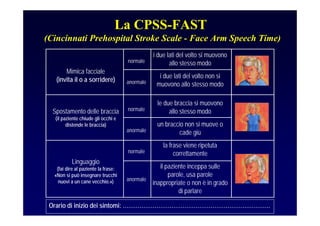
- 22. il paziente inceppa sulle parole, usa parole inappropriate o non ├© in grado di parlare anormale la frase viene ripetuta correttamentenormale Linguaggio (fai dire al paziente la frase: ┬½Non si pu├▓ insegnare trucchi nuovi a un cane vecchio.┬╗) un braccio non si muove o cade gi├╣anormale le due braccia si muovono allo stesso modonormaleSpostamento delle braccia (il paziente chiude gli occhi e distende le braccia) i due lati del volto non si muovono allo stesso modoanormale i due lati del volto si muovono allo stesso modonormale Mimica facciale (invita il o a sorridere) Orario di inizio dei sintomi: ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”. La CPSS-FAST (Cincinnati Prehospital Stroke Scale - Face Arm Speech Time)
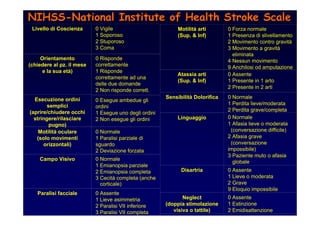
- 23. Livello di Coscienza 0 Vigile 1 Soporoso 2 Stuporoso 3 Coma Motilit├Ā oculare (solo movimenti orizzontali) 0 Normale 1 Paralisi parziale di sguardo 2 Deviazione forzata Campo Visivo 0 Normale 1 Emianopsia parziale 2 Emianopsia completa 3 Cecit├Ā completa (anche corticale) Motilit├Ā arti (Sup. & Inf) 0 Forza normale 1 Presenza di slivellamento 2 Movimento contro gravit├Ā 3 Movimento a gravit├Ā eliminata 4 Nessun movimento 9 Anchilosi od amputazione Esecuzione ordini semplici (aprire/chiudere occhi stringere/rilasciare pugno) 0 Esegue ambedue gli ordini 1 Esegue uno degli ordini 2 Non esegue gli ordini Orientamento (chiedere al pz. il mese e la sua et├Ā) 0 Risponde correttamente 1 Risponde correttamente ad una delle due domande 2 Non risponde corrett. Paralisi facciale 0 Assente 1 Lieve asimmetria 2 Paralisi VII inferiore 3 Paralisi VII completa Atassia arti (Sup. & Inf) 0 Assente 1 Presente in 1 arto 2 Presente in 2 arti Sensibilit├Ā Dolorifica 0 Normale 1 Perdita lieve/moderata 2 Perdita grave/completa Linguaggio 0 Normale 1 Afasia lieve o moderata (conversazione difficile) 2 Afasia grave (conversazione impossibile) 3 Paziente muto o afasia globale Disartria 0 Assente 1 Lieve o moderata 2 Grave 9 Eloquio impossibile Neglect (doppia stimolazione visiva o tattile) 0 Assente 1 Estinzione 2 Emidisattenzione NIHSSNIHSS--NationalNational InstituteInstitute ofof HealthHealth Stroke ScaleStroke Scale
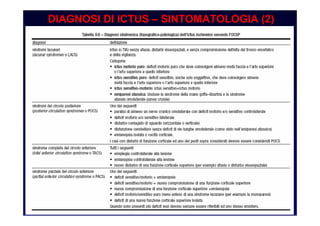
- 24. DIAGNOSI DI ICTUS ŌĆō SINTOMATOLOGIA (2)
- 25. LŌĆÖesame clinico non ├© sufficientemente accurato per differenziare lŌĆÖictus ischemico da quello emorragico in modo assoluto. Per tale distinzione sono necessarie una TC o una RM. DISTINZIONE DEL TIPO DI ICTUS
- 26. TAC cranio di un paziente con ictus ischemico (a sinistra) e di un paziente con ictus emorragico (a destra) DIAGNOSI DI ICTUS ŌĆō NEUROIMMAGINI
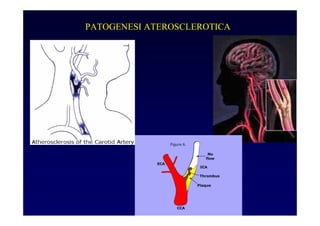
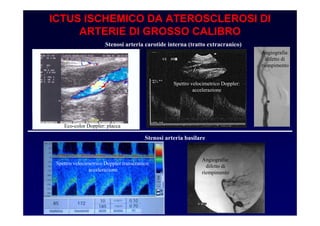
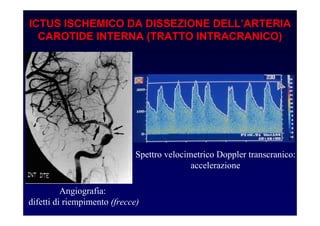
- 27. ICTUS ISCHEMICO DA ATEROSCLEROSI DI ARTERIE DI GROSSO CALIBRO Stenosi arteria carotide interna (tratto extracranico) Stenosi arteria basilare Eco-color Doppler: placca Spettro velocimetrico Doppler: accelerazione Angiografia: difetto di riempimento Angiografia: difetto di riempimento Spettro velocimetrico Doppler transcranico: accelerazione
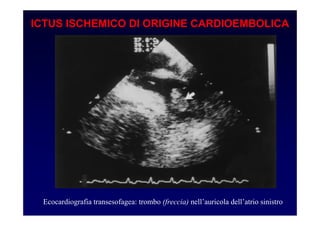
- 28. ICTUS ISCHEMICO DI ORIGINE CARDIOEMBOLICA Ecocardiografia transesofagea: trombo (freccia) nellŌĆÖauricola dellŌĆÖatrio sinistro
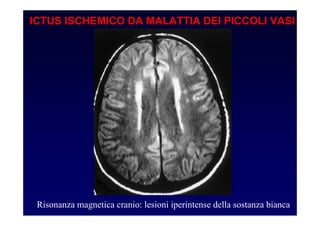
- 29. ICTUS ISCHEMICO DA MALATTIA DEI PICCOLI VASI Risonanza magnetica cranio: lesioni iperintense della sostanza bianca
- 30. ICTUS ISCHEMICO DA DISSEZIONE DELLŌĆÖARTERIA CAROTIDE INTERNA (TRATTO INTRACRANICO) Angiografia: difetti di riempimento (frecce) Spettro velocimetrico Doppler transcranico: accelerazione
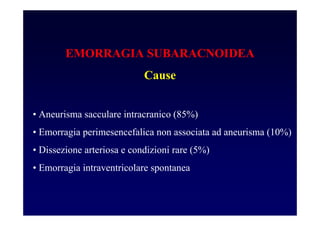
- 33. EMORRAGIA SUBARACNOIDEA Cause ŌĆó Aneurisma sacculare intracranico (85%) ŌĆó Emorragia perimesencefalica non associata ad aneurisma (10%) ŌĆó Dissezione arteriosa e condizioni rare (5%) ŌĆó Emorragia intraventricolare spontanea
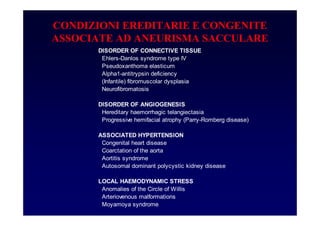
- 34. CONDIZIONI EREDITARIE E CONGENITE ASSOCIATE AD ANEURISMA SACCULARE DISORDER OF CONNECTIVE TISSUE Ehlers-Danlos syndrome type IV Pseudoxanthoma elasticum Alpha1-antitrypsin deficiency (Infantile) fibromuscolar dysplasia Neurofibromatosis DISORDER OF ANGIOGENESIS Hereditary haemorrhagic telangiectasia Progressive hemifacial atrophy (Parry-Romberg disease) ASSOCIATED HYPERTENSION Congenital heart disease Coarctation of the aorta Aortitis syndrome Autosomal dominant polycystic kidney disease LOCAL HAEMODYNAMIC STRESS Anomalies of the Circle of Willis Arteriovenous malformations Moyamoya syndrome
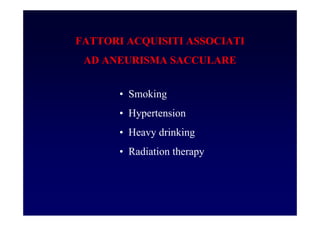
- 35. FATTORI ACQUISITI ASSOCIATI AD ANEURISMA SACCULARE ŌĆó Smoking ŌĆó Hypertension ŌĆó Heavy drinking ŌĆó Radiation therapy
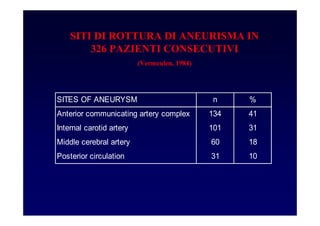
- 36. SITI DI ROTTURA DI ANEURISMA IN 326 PAZIENTI CONSECUTIVI (Vermeulen, 1984) SITES OF ANEURYSM n % Anterior communicating artery complex 134 41 Internal carotid artery 101 31 Middle cerebral artery 60 18 Posterior circulation 31 10
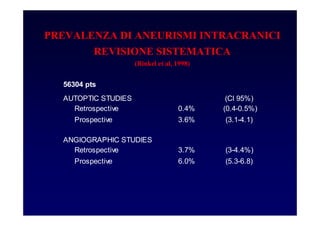
- 37. PREVALENZA DI ANEURISMI INTRACRANICI REVISIONE SISTEMATICA (Rinkel et al, 1998) 56304 pts AUTOPTIC STUDIES (CI 95%) Retrospective 0.4% (0.4-0.5%) Prospective 3.6% (3.1-4.1) ANGIOGRAPHIC STUDIES Retrospective 3.7% (3-4.4%) Prospective 6.0% (5.3-6.8)
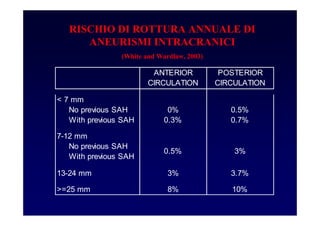
- 38. RISCHIO DI ROTTURA ANNUALE DI ANEURISMI INTRACRANICI (White and Wardlaw, 2003) ANTERIOR CIRCULATION POSTERIOR CIRCULATION < 7 mm No previous SAH 0% 0.5% With previous SAH 0.3% 0.7% 7-12 mm No previous SAH With previous SAH 13-24 mm 3% 3.7% >=25 mm 8% 10% 0.5% 3%
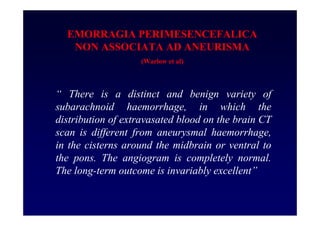
- 39. EMORRAGIA PERIMESENCEFALICA NON ASSOCIATA AD ANEURISMA (Warlow et al) ŌĆ£ There is a distinct and benign variety of subarachnoid haemorrhage, in which the distribution of extravasated blood on the brain CT scan is different from aneurysmal haemorrhage, in the cisterns around the midbrain or ventral to the pons. The angiogram is completely normal. The long-term outcome is invariably excellentŌĆØ
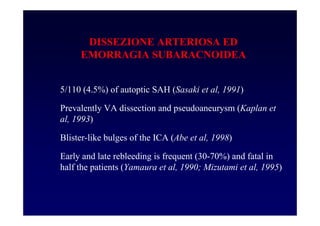
- 40. DISSEZIONE ARTERIOSA ED EMORRAGIA SUBARACNOIDEA 5/110 (4.5%) of autoptic SAH (Sasaki et al, 1991) Prevalently VA dissection and pseudoaneurysm (Kaplan et al, 1993) Blister-like bulges of the ICA (Abe et al, 1998) Early and late rebleeding is frequent (30-70%) and fatal in half the patients (Yamaura et al, 1990; Mizutami et al, 1995)
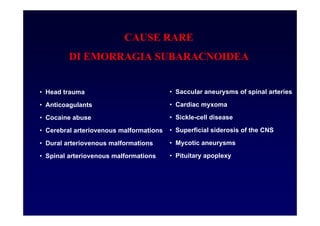
- 41. CAUSE RARE DI EMORRAGIA SUBARACNOIDEA ŌĆó Head trauma ŌĆó Anticoagulants ŌĆó Cocaine abuse ŌĆó Cerebral arteriovenous malformations ŌĆó Dural arteriovenous malformations ŌĆó Spinal arteriovenous malformations ŌĆó Saccular aneurysms of spinal arteries ŌĆó Cardiac myxoma ŌĆó Sickle-cell disease ŌĆó Superficial siderosis of the CNS ŌĆó Mycotic aneurysms ŌĆó Pituitary apoplexy
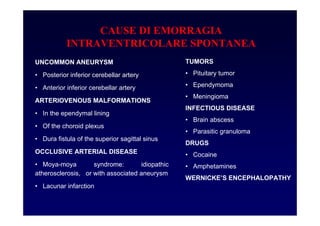
- 42. CAUSE DI EMORRAGIA INTRAVENTRICOLARE SPONTANEA UNCOMMON ANEURYSM ŌĆó Posterior inferior cerebellar artery ŌĆó Anterior inferior cerebellar artery ARTERIOVENOUS MALFORMATIONS ŌĆó In the ependymal lining ŌĆó Of the choroid plexus ŌĆó Dura fistula of the superior sagittal sinus OCCLUSIVE ARTERIAL DISEASE ŌĆó Moya-moya syndrome: idiopathic atherosclerosis, or with associated aneurysm ŌĆó Lacunar infarction TUMORS ŌĆó Pituitary tumor ŌĆó Ependymoma ŌĆó Meningioma INFECTIOUS DISEASE ŌĆó Brain abscess ŌĆó Parasitic granuloma DRUGS ŌĆó Cocaine ŌĆó Amphetamines WERNICKEŌĆÖS ENCEPHALOPATHY
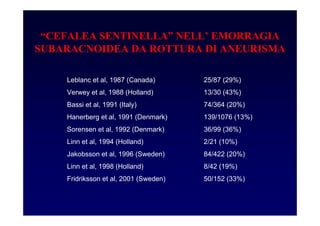
- 43. ŌĆ£CEFALEA SENTINELLAŌĆØ NELLŌĆÖ EMORRAGIA SUBARACNOIDEA DA ROTTURA DI ANEURISMA Leblanc et al, 1987 (Canada) 25/87 (29%) Verwey et al, 1988 (Holland) 13/30 (43%) Bassi et al, 1991 (Italy) 74/364 (20%) Hanerberg et al, 1991 (Denmark) 139/1076 (13%) Sorensen et al, 1992 (Denmark) 36/99 (36%) Linn et al, 1994 (Holland) 2/21 (10%) Jakobsson et al, 1996 (Sweden) 84/422 (20%) Linn et al, 1998 (Holland) 8/42 (19%) Fridriksson et al, 2001 (Sweden) 50/152 (33%)
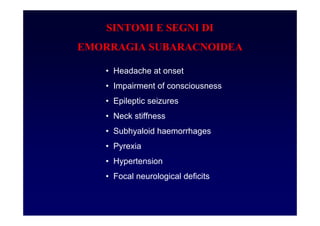
- 44. SINTOMI E SEGNI DI EMORRAGIA SUBARACNOIDEA ŌĆó Headache at onset ŌĆó Impairment of consciousness ŌĆó Epileptic seizures ŌĆó Neck stiffness ŌĆó Subhyaloid haemorrhages ŌĆó Pyrexia ŌĆó Hypertension ŌĆó Focal neurological deficits
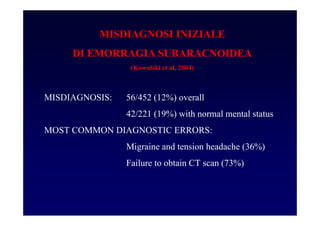
- 45. MISDIAGNOSI INIZIALE DI EMORRAGIA SUBARACNOIDEA (Kowalski et al, 2004) MISDIAGNOSIS: 56/452 (12%) overall 42/221 (19%) with normal mental status MOST COMMON DIAGNOSTIC ERRORS: Migraine and tension headache (36%) Failure to obtain CT scan (73%)
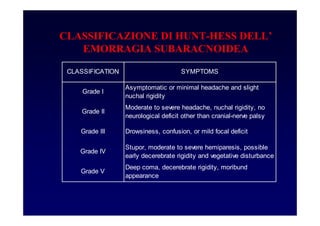
- 46. CLASSIFICAZIONE DI HUNT-HESS DELLŌĆÖ EMORRAGIA SUBARACNOIDEA CLASSIFICATION SYMPTOMS Grade I Asymptomatic or minimal headache and slight nuchal rigidity Grade II Moderate to severe headache, nuchal rigidity, no neurological deficit other than cranial-nerve palsy Grade III Drowsiness, confusion, or mild focal deficit Grade IV Stupor, moderate to severe hemiparesis, possible early decerebrate rigidity and vegetative disturbance Grade V Deep coma, decerebrate rigidity, moribund appearance
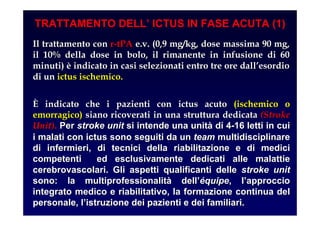
- 47. TRATTAMENTO DELLŌĆÖ ICTUS IN FASE ACUTA (1) Il trattamento conIl trattamento con rr--tPAtPA e.v. (0,9 mg/kg, dose massima 90 mg,e.v. (0,9 mg/kg, dose massima 90 mg, il 10% della dose in bolo, il rimanente in infusione di 60il 10% della dose in bolo, il rimanente in infusione di 60 minuti)minuti) ├©├© indicato in casi selezionati entro tre ore dallindicato in casi selezionati entro tre ore dallŌĆÖŌĆÖesordioesordio di undi un ictus ischemico.ictus ischemico. ├ł├ł indicato che i pazienti con ictus acutoindicato che i pazienti con ictus acuto (ischemico o(ischemico o emorragico)emorragico) siano ricoverati in una struttura dedicatasiano ricoverati in una struttura dedicata (Stroke(Stroke UnitUnit)).. PerPer strokestroke unitunit si intende una unitsi intende una unit├Ā├Ā di 4di 4--16 letti in cui16 letti in cui i malati con ictus sono seguiti da uni malati con ictus sono seguiti da un teamteam multidisciplinaremultidisciplinare di infermieri, di tecnici della riabilitazione e di medicidi infermieri, di tecnici della riabilitazione e di medici competenti ed esclusivamente dedicati alle malattiecompetenti ed esclusivamente dedicati alle malattie cerebrovascolaricerebrovascolari. Gli aspetti qualificanti delle. Gli aspetti qualificanti delle strokestroke unitunit sono: lasono: la multiprofessionalitmultiprofessionalit├Ā├Ā delldellŌĆÖŌĆÖ├®├®quipequipe, l, lŌĆÖŌĆÖapproccioapproccio integrato medico e riabilitativo, la formazione continua delintegrato medico e riabilitativo, la formazione continua del personale, lpersonale, lŌĆÖŌĆÖistruzione dei pazienti e dei familiari.istruzione dei pazienti e dei familiari.
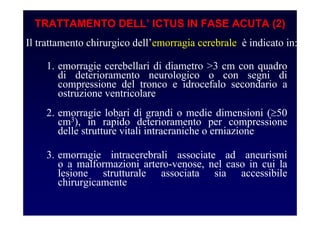
- 48. TRATTAMENTO DELLŌĆÖ ICTUS IN FASE ACUTA (2) Il trattamento chirurgico dellŌĆÖemorragia cerebrale ├© indicato in: 1. emorragie cerebellari di diametro >3 cm con quadro di deterioramento neurologico o con segni di compressione del tronco e idrocefalo secondario a ostruzione ventricolare 2. emorragie lobari di grandi o medie dimensioni (Ōēź50 cm3), in rapido deterioramento per compressione delle strutture vitali intracraniche o erniazione 3. emorragie intracerebrali associate ad aneurismi o a malformazioni artero-venose, nel caso in cui la lesione strutturale associata sia accessibile chirurgicamente
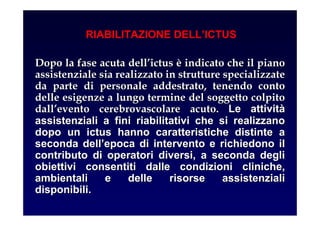
- 49. RIABILITAZIONE DELLŌĆÖICTUS Dopo la fase acuta dellDopo la fase acuta dellŌĆÖŌĆÖictusictus ├©├© indicato che il pianoindicato che il piano assistenziale sia realizzato in strutture specializzateassistenziale sia realizzato in strutture specializzate da parte di personale addestrato, tenendo contoda parte di personale addestrato, tenendo conto delle esigenze a lungo termine del soggetto colpitodelle esigenze a lungo termine del soggetto colpito dalldallŌĆÖŌĆÖevento cerebrovascolare acuto.evento cerebrovascolare acuto. Le attivitLe attivit├Ā├Ā assistenziali a fini riabilitativi che si realizzanoassistenziali a fini riabilitativi che si realizzano dopo un ictus hanno caratteristiche distinte adopo un ictus hanno caratteristiche distinte a seconda dellseconda dellŌĆÖŌĆÖepoca di intervento e richiedono ilepoca di intervento e richiedono il contributo di operatori diversi, a seconda deglicontributo di operatori diversi, a seconda degli obiettivi consentiti dalle condizioni cliniche,obiettivi consentiti dalle condizioni cliniche, ambientali e delle risorse assistenzialiambientali e delle risorse assistenziali disponibili.disponibili.
- 50. PREVENZIONE PRIMARIA DELLŌĆÖICTUS ŌĆóInformazione sullŌĆÖictus ed una educazione a stili di vita adeguati (cessazione del fumo di sigaretta, limitazione del consumo di alcol, attivit├Ā fisica di moderata intensit├Ā, adeguato stile alimentare) ŌĆóTrattamento dellŌĆÖipertensione arteriosa ŌĆóTrattamento della fibrillazione atriale ŌĆóTrattamento del diabete mellito ŌĆóTrattamento dellŌĆÖipercolesterolemia ŌĆóTrattamento anticoagulante in portatori di valvole cardiache meccaniche ŌĆóTrattamento della stenosi carotidea di grave entit├Ā
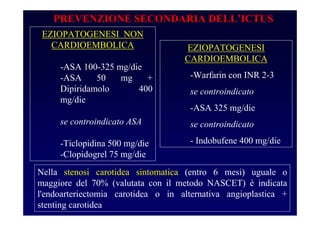
- 51. EZIOPATOGENESI NON CARDIOEMBOLICA -ASA 100-325 mg/die -ASA 50 mg + Dipiridamolo 400 mg/die se controindicato ASA -Ticlopidina 500 mg/die -Clopidogrel 75 mg/die PREVENZIONE SECONDARIA DELLŌĆÖICTUS EZIOPATOGENESI CARDIOEMBOLICA -Warfarin con INR 2-3 se controindicato -ASA 325 mg/die se controindicato - Indobufene 400 mg/die Nella stenosi carotidea sintomatica (entro 6 mesi) uguale o maggiore del 70% (valutata con il metodo NASCET) ├© indicata l'endoarteriectomia carotidea o in alternativa angioplastica + stenting carotidea
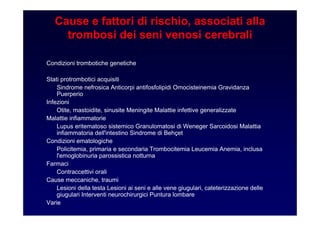
- 53. Cause e fattori di rischio, associati alla trombosi dei seni venosi cerebrali Condizioni trombotiche genetiche Stati protrombotici acquisiti Sindrome nefrosica Anticorpi antifosfolipidi Omocisteinemia Gravidanza Puerperio Infezioni Otite, mastoidite, sinusite Meningite Malattie infettive generalizzate Malattie infiammatorie Lupus eritematoso sistemico Granulomatosi di Weneger Sarcoidosi Malattia infiammatoria dell'intestino Sindrome di Beh├¦et Condizioni ematologiche Policitemia, primaria e secondaria Trombocitemia Leucemia Anemia, inclusa l'emoglobinuria parossistica notturna Farmaci Contraccettivi orali Cause meccaniche, traumi Lesioni della testa Lesioni ai seni e alle vene giugulari, cateterizzazione delle giugulari Interventi neurochirurgici Puntura lombare Varie
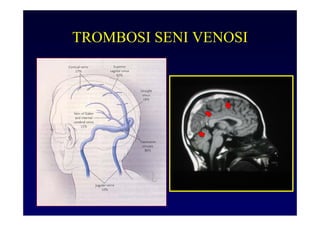
- 54. TROMBOSI SENI VENOSI Clinica: cefalea, vomito, crisi epilettiche, infarti cerebrali Terapia eparina ev seguita da anticoagulanti orali






























![Mechanical thrombectomy in acute stroke [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/mechanicalthrombectomyinacutestrokeautosaved-230102142009-fe15766f-thumbnail.jpg?width=560&fit=bounds)









































