Microbiology Poster Presentation
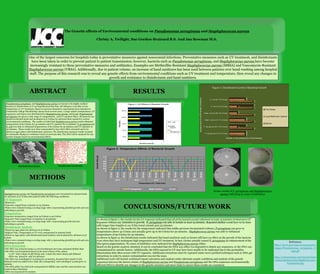
- 1. The Genetic effects of Environmental conditions on Pseudomonas aeruginosa and Staphylococcus aureus Christy A. Twilight, Sue Gordon-Brainard B.S. And Jan Bowman M.S. ABSTRACT METHODS RESULTS Pseudomonas aeruginosa and Staphylococcus aureus are known to be highly resilient bacteria to disinfectants so it was hypothesized that they will still grow even after severe temperature or UV treatment. Based on previous laboratory experiments from Jamestown Community College Microbiology classes from several years, a range relative temperatures, UV exposures, and times were determined for Staphylococcus aureus and E.coli. Pseudomonas aeruginosa was given a wide range of temperatures, and UV exposure times. All bacteria was placed in nutrient broth and incubated at 37 Celsius for 48 hours then exposed to various environmental conditions. The results revealed that Staphylococcus aureus could withstand temperatures of 90 Celsius for 30 minutes and UV exposure for 15 minutes. P. aeruginosa and E. coli were able to withstand temperatures of 60 Celsius for 30 minutes and UV exposure of 25 minutes. These results were then resuspended to have their DNA extracted and to be placed on agar plates with disinfectant exposures. The disinfectant exposure results revealed no noticeable changes in resistance based on previous data. The DNA will be analyzed for any genetic changes based on environmental effects. One of the largest concerns for hospitals today is preventative measures against nosocomial infections. Preventative measures such as UV treatment, and disinfectants have been taken in order to prevent patient to patient transmission; however, bacteria such as Pseudomonas aeruginosa, and Staphylococcus aureus have become increasingly resistant to these preventative measures and antibiotics. Examples are Methicillin-Resistant Staphylococcus aureus (MRSA) and Vancomycin-Resistant Staphylococcus aureus (VRSA). Additionally, due to patient volume, an increase of hand sanitizers has been used between patients over hand washing among hospital staff. The purpose of this research was to reveal any genetic effects from environmental conditions such as UV treatment and temperature, then reveal any changes in growth and resistance to disinfectants and hand sanitizers. As shown in figure 1, the results for the UV exposure indicated that all of the bacteria tested withstood at least 15 minutes of shortwave UV Exposure without any inhibition to growth. P. aeruginosa was able to handle at least 25 minutes. Repeated studies would have to be done with longer time lengths to see if this trend extends past 25 minutes. As shown in figure 2, the results for the temperature indicated that unlike previous documented evidence, P.aeruginosa can grow in temperatures above 42 Celsius and actually grow up to 60 Celsius for 30 minutes. Staphylococcus aureus was able to withstand temperatures of 90 Celsius for 30 minutes. As shown in figure 3, the disinfectant results indicated that hand sanitizers such as Germx still have no effect on the growth of the bacteria even when they have undergone high temperature and UV treatment. In fact, Germx actually caused P. aeruginosa an enhancement of the blue/green pigmentation. No zones of inhibition were indicated for Staphylococcus aureus either. Based on the genetic analysis obtained, it can be concluded that the DNA was either too degraded to obtain any sequences, or the DNA was contaminated by outside factors. Additionally, the DNA exposed to UV may have been unable to be replicated due to the pyrimidine dimerization that often occurs with UV exposure. Additional extractions must be repeated under more purified techniques such as DNA gel extractions in order to ensure contamination was not the issue. Additional work will include continued repeat extraction and analysis under alternate aseptic conditions and analysis of the genetic sequences between the known strains of Staphylococcus aureus and Pseudomonas aeruginosa and the DNA sequences environmentally affected DNA to identify any changes in the genetic structure and more trials to ensure these results are consistent. CONCLUSIONS/FUTURE WORK Staphylococcus aureus and Psuedomonas aeruginosa were inoculated in nutrient broth for 48 hours at 37 Celsius then placed under the following conditions: UV Exposure •Shortwave •Exposure ranged from 5 minutes to 25 minutes •Plates were evaluated using a scoring range with 2 representing plentiful growth and zero indicating no growth . Temperature •Exposure temperature ranged from 50 Celsius to 90 Celsius •Exposure Time ranged from 10 minutes to 30 minutes •Plates were evaluated using a scoring range with 1 representing growth and zero indicating no growth. Disinfectant Analysis •Placed on Agar plates for 48 hours at 37 Celsius •Highest Time, Temperature or UV were resuspended in nutrient broth •Plated on Agar plates with disinfectant/hand sanitizer and incubated for 48 hours at 37 Celsius •Plates were evaluated using a scoring range with 3 representing plentiful growth and zero indicating no growth. DNA Extraction •The DNA was extracted using 2-3 ml of isobutanol and water saturated diethyl ether •The DNA was Precipitated based on the total volume of the culture •1/10th total volume of 3M NaOAc and 2 times the total volume 95% Ethanol •DNA was placed in -20C for 48 hours •The DNA was centrifuged at 12,000xg for 15 minutes, decanted then 200ul of 75% Ethanol wash was added twice while also resuspended and centrifuged 12,000xg for 10 minutes •The DNA pellet was dried and resuspended in MilliQ water and the concentration was tested using a Nanodrop •DNA was sequenced for analysis Staphylococcus aureus Pseudomonas aeruginosa 0 0.2 0.4 0.6 0.8 1 1.2 10min 20min 30min 10min 20min 30min 10min 20min 30min 10min 20min 30min 10min 20min 30min 50 C 60 C 70 C 80 C 90 C Growth(Visual) Temperature (C) Time (min) Figure 2: Temperature Effects of Bacterial Growth P. aeruginosa Staph. aureus E. coli 0 1 2 3 8min 10min 15min 20min 25min Growth (visual) Time(min) Figure 1: UV Effects of Bacterial Growth E. coli Staph. aureus P. aeruginosa strain 60 C 70 C 80 C 90 C 10min 20min 30min 10min 20min 30min 10min 20min 30min 10min 20min #27853 - - - - - - - - - - + #25923 < < < < < < - - - + - < < < - - - < < - < < + - < + + + + + + + - - + + + + + - + + - - - - - strain 8min 10min 15min 20min 25min Name Germx Lysol Bathroom cleaner P. aeruginosa UV 25 minutes 2 2 #27853 + + + + + P. aeruginosa 60 C 30 minutes 3 1 #25923 ++ ++ ++ - - Staph. aureus UV 15 minutes 3 2 ++ ++ ++ ++ ++ Staph. aureus 90C 20 minutes 3 1 E. coli UV 25 minutes 3 1 ++ E. coli 60C 30 minutes 3 2 2 3 3 3 3 3 2 1 2 1 1 2 2 2 2 1 3 2 P. aeruginosa UV 25 minutes P. aeruginosa 60 C 30 minutes Staph. aureus UV 15 minutes Staph. aureus 90C 20 minutes E. coli UV 25 minutes E. coli 60C 30 minutes Growth in the presence of Disinfectant BacteriaandEnvironmentalConditions Figure 3: Disinfectant Control of Bacterial Growth The Works Lysol Bathroom cleaner Germx Germx results of P. aeruginosa and Staphylococcus aureus indicating no zones of inhibition References http://www.marvistavet.org/assets/i mages/Pseudomonas_aeruginosa_G ram.gif http://entomologia.net/insectos%20 contra%20bacterias/Staphylococcus %20aureus.jpg