Editor's Notes
- #4: Diabetes foot disease is the most common cause of non-traumatic lower-limb amputation globally. However, most foot problems are preventable through early detection of the problem and prompt treatment by a skilled multidisciplinary healthcare team.
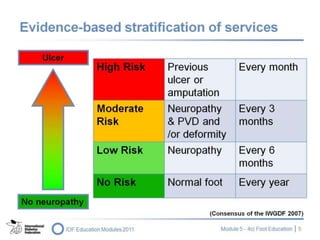
- #5: Different people with diabetes require different levels of foot education. This is because there is a wide range to levels of foot risk. This needs to be taken into consideration when providing foot education programmes. We know that living with diabetes is not easy; people with diabetes must assimilate a great deal of information and complete a series of daily tasks in order to effectively self-manage their condition. Lifestyle and behavioural changes regarding the feet, therefore, should be required only from people who are at high risk ŌĆō i.e. people with decreased sensation and/or blood flow in lower limbs.
- #6: No country has the resources to provide comprehensive foot care to all people with diabetes. Therefore, a system has been developed for stratifying services based on levels of risk. This system is used widely around the world. We should stratify people with diabetes according to their level of risk ŌĆō from low risk to very high risk.
- #7: Note to the educator: Ask participants briefly to try to predict the content of the following slide ŌĆō the different (in terms of risk) people with diabetes who should be targeted for foot care education. Ask what kind of education they think will be required.
- #8: The people at low risk are those who have normal sensation in both feet and normal blood flow. These people need simple advice. They need an annual foot assessment. People at high risk have decreased sensation, and have at some point had an ulcer or have peripheral vascular disease. These people need intensive education that involves practical demonstrations. Everyone should be cautioned about walking barefoot and should be taught to wash and examine their feet every day. Because many of us as healthcare providers have experienced the traditional medical model of learning, we think it is important to teach people about neuropathy and vascular disease; in fact, we should focus on teaching people how to avoid situations that cause ulcers. Research findings from around the world demonstrate that ill-fitting shoes are the most common cause of ulceration ŌĆō the cause of about 60% of new ulcers.
- #9: Note to the educator: Again, ask participants to quickly brainstorm ideas before moving on to the next slide.
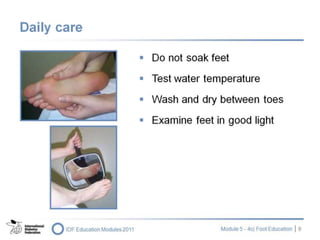
- #10: People must learn to wash, touch and look at their feet every day. Soaking feet is not recommended as it dries out the natural oils in the skin. Because most of these people have no sensation at all in their feet, it is imperative that they learn how to: Test water temperature with their hands or elbows ŌĆō surprising number of people put their feet in boiling water, causing burns Examine feet under good light ŌĆō many people may have diabetes-related eye damage Wipe feet using a light-coloured towel ŌĆō any blood or pus will show on the towel Make sure the spaces between the toes are dried properly as moisture can lead to macerations and infections Inspect all parts of the feet Feel around every toenail for sharp edges ŌĆō these can cut into the adjacent toe, causing ulceration Learn to use a mirror to check their feet and/or ask a family member to assist
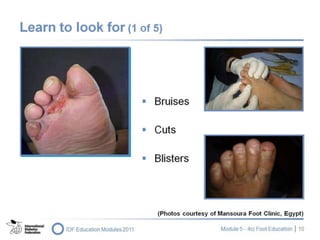
- #11: People should look for bruises, cuts, blisters or any marks that have recently appeared. Note the importance of checking between toes. The cause of any problems should be investigated Bruises are caused by a number of factors ŌĆō trauma from shoes and/or something falling on top of the foot, for example; a shoe that is too tight in the toe can cause bruising under the toenail, causing it to turn black Cuts can be caused by walking barefoot, stepping on something, or by a sharp seam or stone in the shoe Blisters are often caused by new shoes that are too tight, heaters, electric blankets or foot spas When peopleŌĆÖs feet do not perspire due to autonomic neuropathy they become very dry; it is therefore important to check for dry feet. The dryness can cause cracks, and result in infection Callus (and corns) ŌĆō hard skin that develops in an area of pressure ŌĆō might be caused by an over-tight shoe or the biomechanics of the personŌĆÖs foot; a build up of callus needs immediate attention A hot spot could be a sign of infection ŌĆō which people with nerve damage do not feel Discoloration or swelling might be the sign of a fracture A sharp toenail can dig into an adjacent toe, provoking ulceration An ingrown toenail, caused by a toenail that has not been cut properly, provokes redness and swelling around the nail. If the spaces between the toes are not dried properly after washing, the skin can turn soggy and lead to infection
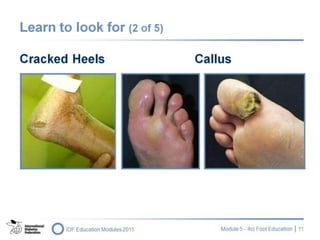
- #12: People should check their heels. Peripheral neuropathy also involves autonomic neuropathy, which results in impaired perspiration in the feet. The skin dries out and becomes cracked. Those cracks could become a portal for infection. An example of cracked heels is shown on this slide. People should also look at callus. In neuropathy, the intrinsic muscles of the foot are weakened. This causes the toes to become clawed and the fat pads under the foot to move forward. People thus walk on the bones of their feet, provoking further formation of callus. Although it is sometimes perceived as protective, in people with diabetic foot, callus is very dangerous. Ask participants to look closely at the callus on the right-hand side of the slide. This is called a ŌĆśhaemorrhagicŌĆÖ callus. The person has continued walking on this large callus without changing the way she walked. The tissue under the callus has broken down and bled into the callus. If at this point this callus were to be removed, an ulcer might be found underneath. If people have cracked heels (left), they need to have the skin removed by sharp debridement. Creams would be ineffective at this stage. These sort of cracks and dry skin are usually caused through the use of open-back sandals and walking barefoot. People should wear shoes with an enclosed heel and apply cream regularly as a preventive measure.
- #13: Due to biomechanical (structural) changes to the foot, people might develop hammer toes. This kind of toe does not fit easily in a shoe. As a result, the tip and the top of the toe become perfect areas for the development of corns and calluses and can subsequently be a site for ulceration. Similarly, clawed toes are a problem because pressure is concentrated on the tips of the toes. Again, as a result, there is a build up of callus. Because the toes are clawed, there is a lack of ventilation. This leads to problems of maceration between the digits. Therefore, people should be advised to dry carefully between the toes.
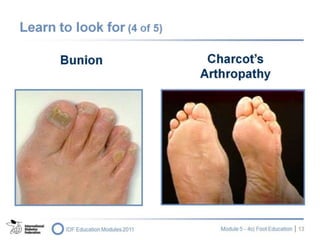
- #14: Any foot that is deformed ŌĆō such as a foot with bunions (left) can lead to problems: a bunion fits into shoes with difficulty. This area of the foot can rub on the shoe, leading to ulceration. CharcotŌĆÖs arthropathy (right, the mid-foot in this case has collapsed) causes severe deformity. It is very difficult for this sort of foot to fit into a normal shoe. Looking at the foot on the left, we can see a corn on the top of the fourth digit which was probably caused by a shoe that was too tight at the toe. People require shoes ŌĆō from a specialized orthopaedic footwear dealer ŌĆō that are wide and deep enough to accommodate foot deformities. People should be aware of the need to check bunions for redness and hard skin. Corns should be removed by someone who is skilled in sharp debridement.
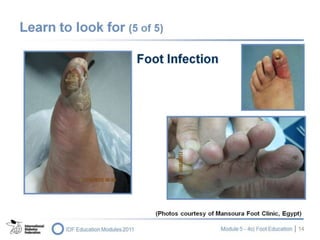
- #15: Redness and swelling is a sign of infection. Remember, people with diabetes foot complications cannot feel pain. People should look for any infection. This involves looking underneath as well as on the top of the feet. Foot infection is the most under-recognized and under-treated problem in people with diabetes. The lower right picture shows tinea pedis.
- #16: People should learn to care for their skin. Remember what was said earlier: with autonomic neuropathy, people lose the ability to perspire and the skin becomes dry. It is recommended that people apply cream on their feet every day. In this way, both the hands and the eyes are used to check the feet. It is important that cream is rubbed in all over the feet but not between the toes and not in open sores. Avoid using herbal treatments and ointments when the ingredients are unknown. Urea-based cream is beneficial for cracked heels.
- #17: Cutting toenails is an important issue. The correct way to do this is to cut the toenails with clippers. People should not allow nails to grow too long and should always cut nails straight across the end. People are advised to check for sharp edges and use a file where necessary to reduce sharpness. People who are at high risk should have their nails cut by a podiatrist. However, this is not always possible. Family members should learn how to help with toenail cutting and checking feet. If nails are thick, these should be reduced ŌĆō the thick nail can cause ulceration. If nails are thickened and/or crowded, such as in the lower left photo, people should have help in cutting them.
- #18: Tinea (athleteŌĆÖs foot) is one of the most common causes of cellulitis in people with diabetes. When carrying out a foot assessment, it is very important to check between the toes to make sure there is no tinea or soggy skin and check for any signs of tinea around the foot. Tinea can appear as small brown or red spots, small (water-filled) blisters, soggy, flaky skin between toes. Note: people cannot feel itchiness. To treat this, people should learn to use a powder between their toes, rather than a cream or lotion. People should use a cream on the foot itself. It is most important that the surrounding area be treated until the infection goes away. People should wash socks regularly and hang them out to dry where possible. Showers and baths should be treated and cleaned. Family members who use the same shower should be checked for tinea so that this can be treated and further infection prevented. Outside the home, people should use flip-flops (rubber sandals or thongs) in the shower to prevent tinea infection.
- #19: Many people with diabetes develop fungal nails. These can be difficult to treat and, apart from being unsightly, the major problem with fungal nails is that they can become very thick. If these thickened toenails go into a shoe that is too tight-fitting, excessive pressure can be placed on the nail of the big toe and an ulcer can occur under the nail. It is important that these thick nails are filed down. Nail scrapings can be carried out by a podiatrist or doctor; appropriate treatment can be prescribed for the nail infection.
- #20: People should be careful when buying socks. It is most important to choose the correct size. Socks that are too small reduce the blood circulation; socks that are too big create extra pressure. Socks warm the feet, absorb sweat, and prevent friction so that blisters are less likely to occur. Wool or cotton or a wool/cotton mix are preferable, but socks with 20% to 30% synthetic material are almost as good. Padded socks, as long as they allow the foot to fit comfortably in the shoe, can reduce pressure. Elastic around the leg should not be too tight as this cuts in to the leg and reduces circulation. Women should not use anklets or knee-high stockings. Check for rough seams in the socks ŌĆō these can cause ulceration. Avoid socks with a lot of patterns ŌĆō the toes can get caught in the threads in the sock. Socks should be washed and changed every day.
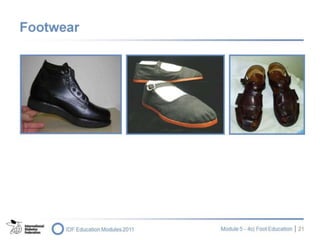
- #21: Below are some important shoe-related issues. Shoes should be wide and deep at the toe, enabling a foot with clawed toes and bunions to fit easily; the shoe should be 1 cm to 1.5 cm longer than the foot Shoes should have a thick rubber sole; a leather sole is not advisable High heels are not recommended as they put too much pressure on the forefoot The back of the shoe, the ŌĆśheel counterŌĆÖ, should be firm enough to provide support for the foot To cope with swelling, shoes should have a lace-up or velcro fastening; this helps to keep the foot firmly in the shoe It is important to feel inside the shoe; if there are any rough seams, the insensate foot will not feel them and the person will continue to wear the shoe until an ulcer develops Leather shoes are best, as leather absorbs moisture and adapts to the feet; rubber boots should be avoided. Safety boots must be fitted carefully Sometimes, shoes are not enoughŌĆöthe feet might need further deflection and an insole/orthosis might be needed; this requires a podiatrist or a person who is specialized in this field. The shoes must be able to accommodate this device.
- #22: The shoe on the left is an example of the footwear that people with diabetes in Australia are advised to wear. People are recommended to wear something on their feet every time the foot hits the ground; socks are not enough. People can wear a kind of sandal (right) or shoe (middle). These provide some protection and are better than nothing at all. People with foot deformities need specially made shoes.
- #23: Below are some recommendations when buying shoes. To avoid choosing a shoe that is too tight, people should buy shoes in the afternoon, when feet are naturally more swollen Both feet should be measured with the person standing ŌĆō a person can have feet of different sizes. It is important to note that shoe manufacturers use different size systems It is also important to explain to people that they may not be able to feel pain or pressure if the shoe is too small. Where possible, people should be advised to show new shoes to a foot care specialist so that the shoes and the fit can be checked. People should not wear new shoes for long periods of time. They should wear the shoes at home for 30 minutes and then take off shoes and socks to make sure that no red marks or rubs have been provoked on their feet. The wearing time should be extended until the shoe can be worn almost all day. When this has been done for two or three days, the shoes can be worn outdoors. Shoes must be worn at all times. It is important to have slippers next to the bed in case people have to get up during the night.
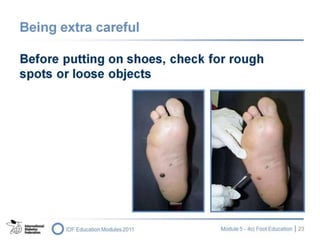
- #24: It is common for things to fall into shoes. In the photographs on this slide, the man had stepped on a nail. It was only when he attended a foot clinic and his shoes were taken off that he realized he had a nail driven into the sole of his foot. It is very important that before they put their shoes on, people with insensate feet use their hands to check inside for any loose objects and inspect their feet daily. Shoes should be shaken before wearing. The soles should be inspected; if worn down, they can be slippery.
- #25: People with insensate feet are subject to burns caused by the sun or external sources of heat such as hot water bottles or heaters. People are advised to apply sun block on their feet if the skin is exposed. Some people have the sensation that their feet are cold and put them near a heater. As a result, many people suffer burns on their feet. They should ensure that their feet remain at least 3 m from heaters. Electric blankets should be turned off before people go to bed. People should not use hot-water bottles or walk barefoot.
- #26: People whose feet are at high risk should not be advised to do more walking than is necessary for daily living. These people should avoid weight-bearing exercises. They can do non-weight-bearing exercises and should be advised to swim, or ride an exercise bike.
- #27: It is important for written material to be written at the right reading and comprehension level. Large fonts should be used to enable people with visual impairment to read the material. Pictures should be relevant to the text and support learning ŌĆō not simply be decorative.
- #28: All education programmes should be evaluated in order to assess usefulness and learning value. The key lies in evaluating behavioural changes. It is important, therefore, to ask the following kinds of questions: 'How many times have you checked your feet this week?ŌĆÖ ŌĆśHow many times have you put cream on your feet in the previous week?ŌĆÖ The behavioural changes reflected in the answers to these questions are far more important than a knowledge of the signs and symptoms of neuropathy.
- #29: The key messages of this presentation are: Not everybody with diabetes carries the same risk for foot ulceration and amputation Target and educate those people who are at high risk ŌĆō with reduced sensation and reduced blood flow Shoes are the most common cause of ulceration; this should be the focus of any foot care education programme People need to learn to identify any problems that occur early on and advise a healthcare provider where possible Most importantly, health professionals need to be specially trained in caring for people with diabetic foot disease People working in foot care should be encouraged to develop a special interest group in this very important area to share knowledge and best practices