RESPIRATORY DISTRESS IN NEWBORN final.pptx
- 1. RESPIRATORY DISTRESS IN NEWBORN By : Ashwin Kumar
- 2. ŌĆó B/O Nancy, baby boy born via SVD at 38 weeks with birth weight 3kg ŌĆó Mother is 39 year old, para 4, with anemia in pregnancy ŌĆó She presented with contraction pain and fever 1 day before the delivery, her UFEME showed leucocyte 2+, nitrate negative and she was started on cephalexin for 3 days (TWC 6.51, plt 305), MotherŌĆÖs HVS no growth ŌĆó Subsequently progress into labor and baby born vigorous with good AS (9/10/10) ŌĆó However baby was tachypnea with labile saturation (Spo2 88-90% under room air) at nursery and started on nasal prong at around 2 hours of life and worsening respiratory distress with tachypnea, retractions, and grunting at 4 hours of life and was intubated. Case scenario
- 3. ŌĆó Presumed sepsis ŌĆó Congenital pneumonia ŌĆó Transient tachypnea of newborn (TTN) ŌĆó Persistent pulmonary hypertension of newborn (PPHN) ŌĆō primary or secondary ŌĆó RDS/ hyaline membrane ŌĆó Congenital heart disease ŌĆó Congenital diaphragmatic of hernia Differential diagnosis of respiratory distress in newborn?
- 4. ŌĆó On examination, patient was intubated, tachypnea with recession, good perfusion, other neonatal examinations are normal ŌĆó Lungs clear, equal a/e, CVS DRNM, PA soft ŌĆó BP stable, SPO 100% under low ventilator settings (Pr 18/6, FiO2 30%) ŌĆó FBC normal (TWC 24 (NEU 69.6 %/Lym 15 %)/ HB 20.6/PLT 198/HCT 66.4) ŌĆó ABG : ph. 7.32/Pco2 38/PO2 99 /HCO3 19.6/BE -6.0 ŌĆó CRP : 2.2 ŌĆó Bedside ECHO: TR jet , balanced chamber size, good contractibility Case scenario
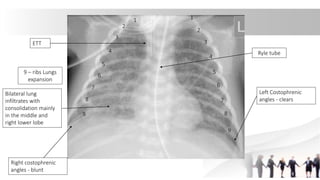
- 5. Case scenario ETT Ryle tube 9 ŌĆō ribs Lungs expansion Bilateral lung infiltrates with consolidation mainly in the middle and right lower lobe Left Costophrenic angles - clears 1 2 3 4 5 6 7 8 9 Right costophrenic angles - blunt 1 2 3 4 5 6 7 8 9
- 6. Differential Differential Point support Point against Congenital pneumonia Mother has fever and UTI Respiratory distress CXR Presumed sepsis Mother has fever and UTI Respiratory distress CXR ŌĆō no obvious consolidation Transient tachypnea of newborn Respiratory distress Respiratory distress at 4 hours of life TTN usually right after birth More commonly seen in LSCS CXR not characteristic for TTN Persistent pulmonary hypertension of newborn Respiratory distress Labile Saturation Stable under low ventilator setting ECHO ŌĆō normal Congenital heart disease Respiratory distress Labile Saturation ECHO normal Congenital diaphragmatic of hernia Respiratory distress CXR- no evidence of CDH
- 7. ŌĆó Treated as congenital pneumonia ŌĆó Treatment - Ventilated for 3 days and successfully extubated to nasal prong - Not require inotropes throughout the admission - Completed IV ampicillin and gentamicin for 5 days, blood culture NG - Started feeding at day 1 of life and achieved full feeding Progress
- 9. Objectives ŌĆó Recognize newborn with respiratory distress ŌĆó Understand the differential diagnosis of RDS ŌĆó Learn the pathophysiology, presentation diagnosis and management for the most common causes
- 10. You have called to labour room to review a term baby who is tachypnoea soon after delivery
- 11. ŌĆó Transient tachypnea of newborn (TTN) ŌĆó Congenital pneumonia ŌĆó Respiratory distress syndrome (RDS) ŌĆó Meconium aspiration syndrome (MAS) ŌĆó Persistent pulmonary hypertension of newborn ŌĆó Pneumothorax ŌĆó Congenital heart disease ŌĆó Congenital diaphragmatic of hernia ŌĆó Congenital lung malformation Differential diagnosis
- 12. ŌĆó How old ŌĆó Gestational age (Preterm, term/ post date) ŌĆó Mode of delivery (SVD? LSCS?) ŌĆó Risk factors for sepsis ? Antibiotic given? ŌĆó Antenatal history ŌĆó HVS result? GBS ? ŌĆó Amniotic fluid (Clear? Meconium? ŌĆó CTG, fetal heart rate Take relevant history
- 13. ŌĆó Nasal flaring ŌĆó Tachypnoea, RR > 60 ŌĆó Subcostal, intercostal recession ŌĆó Grunting ŌĆó Cyanosis ŌĆó Lethargy Signs of respiratory distress
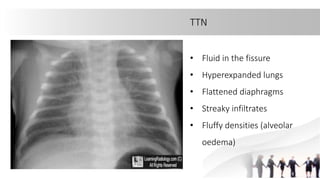
- 14. TTN ŌĆó Most common aetiology ŌĆó Impaired clearance of fetal fluid from lungs at birth ŌĆó Infant born via caesarean section ŌĆó Typically present right after birth ŌĆó Treatment: Respiratory support ŌĆó Resolved 48-72 hours (6 hours)
- 15. TTN ŌĆó Fluid in the fissure ŌĆó Hyperexpanded lungs ŌĆó Flattened diaphragms ŌĆó Streaky infiltrates ŌĆó Fluffy densities (alveolar oedema)
- 16. Congenital pneumonia ŌĆó Tend to be more sick (poor feeding, apnoea, poor perfusion, tachycardia) ŌĆó Present of risk factor: Infant of GBS carrier mother, maternal chorioamnionitis, maternal pyrexia, leaking > 18 hours ŌĆó Investigations: raised TWC, Low plt, raised CRP ŌĆó Treatment: respiratory support, antibiotic, nutrition
- 17. Congenital pneumonia ŌĆó Consolidation with air bronchograms ŌĆó Poor lungs expansion
- 18. RDS ŌĆó Most commonly seen in premature baby ŌĆó Surfactant deficiency in immature lung (Surfactant decrease alveolar surface tension which helps with alveolar expansion and decrease risk of atelectasis. ŌĆó Risk: Extreme premature, no/incomplete antenatal steroid
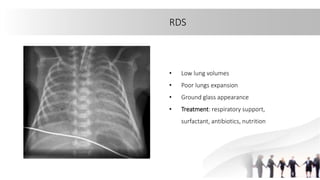
- 19. RDS ŌĆó Low lung volumes ŌĆó Poor lungs expansion ŌĆó Ground glass appearance ŌĆó Treatment: respiratory support, surfactant, antibiotics, nutrition
- 20. Meconium aspiration syndrome ŌĆó Risk factor: Post date, sepsis, stress (any cause of fetal hypoxia) ŌĆó Aspiration of meconium into the lungs ’āĀ Obstruction of airways ’āĀ air trapping ’āĀ alveolar rupture ŌĆó Deactivation and decrease synthesis of surfactant ŌĆó Risk of develop PPHN
- 21. MAS ŌĆó Hyperinflation ŌĆó Flattened diaphragms ŌĆó Diffuse, patchy opacities ŌĆó Treatment: Respiratory support
- 22. Quiz 1 Congenital pneumonia TTN MAS Pneumothorax Congenital heart disease (TGA) CDH RDS Congenital lung malformation
- 23. Quiz 2 You receive another call from O&G to review a newborn in the labour room with tachypnoea.
- 24. Quiz 2 What history you would like to know? Describe what you see What is your differential diagnosis ? What is your management?
- 25. Quiz 3 1 2 3 4 5 Stridor Wheezing Grunting in respiratory distress infant Infant making constipated grunting sounds. Infant grunting while pooping
- 26. Summary ŌĆó Identify the high risk group (Prem delivery, MMSL/TMSL, maternal risk of sepsis etc) ŌĆó Recognize signs and symptoms of respiratory distress ŌĆó NRP ŌĆó Always call for help ŌĆó Early Respiratory support ŌĆó Other treatment will depend on the respective pathologies
- 27. REFERENCES 1. Nelson Textbook Of Paediatrics 2. https://emedicine.medscape.com/article/976914-overview#a7 3. Ncbi: Respiratory Distress of Newborn 4. American Academy of Family Physicians: Respiratory Distress in the Newborn 5. Michael D. Nissen, Congenital and neonatal pneumonia, Paediatric Respiratory Reviews, Volume 8, Issue 3, 2007, Pages 195-203, ISSN 1526-0542, https://doi.org/10.1016/j.prrv.2007.07.001. 6. Pediatric Protocol 7. OPENPediatrics
Editor's Notes
- #4: Ask the floor to name at least 7 of the differential
- #7: Quite obvious for this case The baby has congenital pneumonia With the history of mother having fever and UTI LetŌĆÖs look at other differential diagnosis Basically all will present with respiratory distress With that Im going to talk about the RDS in newborn
- #11: While on your way to labour room, you should have some differential in your mind as you are dealing with a newborn with respiratory distress WhatŌĆÖs the differential in your mind?
- #14: Describe what can see from this video
- #15: Describe what can see from this video
- #16: Describe what can see from this video
- #18: CXR as mentioned earlier
- #19: Surfactant decrease alveolar surface tension Helps with alveolar expansion And decrease risk of atestasis.
- #20: Surfactant decrease alveolar surface tension Helps with alveolar expansion And decrease risk of atestasis.
- #21: Surfactant decrease alveolar surface tension Helps with alveolar expansion And decrease risk of atestasis.
- #22: Surfactant decrease alveolar surface tension Helps with alveolar expansion And decrease risk of atestasis.
- #25: SVD 38 week EFW 3kg ANC ŌĆō fever, tachycardic high TWX, cover with triple antibiotic , 3doses and progress into labour HVS ŌĆō GBS Liquor clear AS 9/9 , CTG normal prior to deliver
- #26: Try to appreciate this sound and interpret the sound
- #27: Surfactant decrease alveolar surface tension Helps with alveolar expansion And decrease risk of atestasis.