Cvp central venous pressure monitoring
- 1. Central Venous Pressure Monitoring ÓĖÖÓĖ▓ÓĖćÓĖ¬ÓĖ▓ÓĖ¦ÓĖøÓĖ┤ÓĖóÓĖŻÓĖ▒ÓĖĢÓĖÖÓ╣ī ÓĖ¦ÓĖćÓĖäÓ╣īÓĖ½ÓĖÖÓĖ▓ÓĖóÓ╣éÓĖüÓĖÅ ÓĖ×ÓĖóÓĖ▓ÓĖÜÓĖ▓ÓĖźÓĖ¦ÓĖ┤ÓĖŖÓĖ▓ÓĖŖÓĖĄÓĖ× ÓĖøÓĖÄÓĖ┤ÓĖÜÓĖĢÓĖ┤ÓĖćÓĖ▓ÓĖÖÓĖŚÓĖĄÓ╣ł ICU trauma ÓĖ▒
- 2. ÓĖéÓ╣ēÓĖŁ ÓĖÜÓ╣łÓĖć ÓĖŖÓĖĄÓ╣ēÓ╣ā ÓĖÖÓĖüÓĖ▓ÓĖŻ monitor CVP ÓĖĪÓĖĄ ÓĖöÓĖ▒ÓĖć ÓĖÖÓĖĄÓ╣ē ’éŚ1.╠² Ó╣āÓĖÖÓĖ£ÓĖ╣ÓĖøÓ╣łÓĖ¦ÓĖóÓĖŚÓĖĄÓ╣łÓĖ¬ÓĖŹÓ╣ĆÓĖ¬ÓĖĄÓĖóÓ╣ĆÓĖźÓĖĘÓĖŁÓĖöÓĖłÓĖ▓ÓĖüÓĖŁÓĖĖÓĖÜÓĖĢÓĖ┤Ó╣ĆÓĖ½ÓĖĢÓĖĖÓĖ½ÓĖŻÓĖĘÓĖŁ Ó╣ē ÓĖ╣ ÓĖ▒ ÓĖłÓĖ▓ÓĖüÓĖüÓĖ▓ÓĖŻÓĖ£Ó╣łÓĖ▓ÓĖĢÓĖ▒ÓĖö ÓĖĀÓĖ▓ÓĖ¦ÓĖ░ sepsis Ó╣üÓĖźÓĖ░ÓĖüÓĖŻÓĖōÓĖĄÓĖŁÓĖĘÓ╣łÓĖÖÓĖŚÓĖĄÓ╣łÓĖŚÓĖ│ÓĖ▓ ’éŚÓ╣āÓĖ½Ó╣ēÓĖøÓĖŻÓĖ┤ÓĖĪÓĖ▓ÓĖōÓ╣ĆÓĖźÓĖĘÓĖŁÓĖöÓ╣üÓĖźÓĖ░ÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣āÓĖÖÓĖŻÓ╣łÓĖ▓ÓĖćÓĖüÓĖ▓ÓĖóÓĖźÓĖöÓĖźÓĖć ’éŚ2.╠² Ó╣āÓĖÖÓĖ£ÓĖ╣ÓĖøÓ╣łÓĖ¦ÓĖóÓĖŚÓĖĄÓ╣łÓĖĪÓĖĄÓĖĀÓĖ▓ÓĖ¦ÓĖ░ÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣ĆÓĖüÓĖ┤ÓĖÖ Ó╣ē ’éŚ3.╠² Ó╣āÓĖÖÓĖüÓĖŻÓĖōÓĖĄÓĖŚÓĖĄÓ╣łÓĖĢÓ╣ēÓĖŁÓĖćÓĖüÓĖ▓ÓĖŻÓĖøÓĖŻÓĖ░Ó╣ĆÓĖĪÓĖ┤ÓĖÖÓĖüÓĖ▓ÓĖŻÓĖŚÓĖ│ÓĖ▓ÓĖćÓĖ▓ÓĖÖÓĖéÓĖŁÓĖć ÓĖ½ÓĖ▒ÓĖ¦Ó╣āÓĖłÓ╣üÓĖźÓĖ░ÓĖ½ÓĖźÓĖŁÓĖöÓ╣ĆÓĖźÓĖĘÓĖŁÓĖö
- 3. Central Venous Pressure (CVP) ’éŚÓĖ½ÓĖĪÓĖ▓ÓĖóÓĖ¢ÓĖČÓĖć ÓĖäÓĖ¦ÓĖ▓ÓĖĪÓĖöÓĖ▒ÓĖÖÓ╣āÓĖÖÓĖ½ÓĖźÓĖŁÓĖöÓ╣ĆÓĖźÓĖĘÓĖŁÓĖöÓĖöÓĖ│ÓĖ▓ Superior Vena Cava (SVC) ÓĖŗÓĖČÓ╣łÓĖćÓĖĪÓĖĄÓĖäÓ╣łÓĖ▓Ó╣ĆÓĖŚÓ╣łÓĖ▓ÓĖüÓĖ▒ÓĖÜÓĖäÓĖ¦ÓĖ▓ÓĖĪÓĖöÓĖ▒ÓĖÖÓĖéÓĖŁÓĖć right atrium (RA) Ó╣üÓĖźÓĖ░Ó╣ĆÓĖøÓ╣ćÓĖÖÓĖüÓĖ▓ÓĖŻÓ╣üÓĖ¬ÓĖöÓĖćÓĖ¢ÓĖČÓĖć preload ÓĖéÓĖŁÓĖć right ventricle (RV) ÓĖ½ÓĖŻÓĖĘÓĖŁ right ventricular end-diastolic pressure (RVEDP) ÓĖäÓ╣łÓĖ▓ CVP ÓĖłÓĖ░ÓĖÜÓĖŁÓĖüÓ╣äÓĖöÓ╣ēÓĖ¢ÓĖČÓĖćÓĖøÓĖŻÓĖ┤ÓĖĪÓĖ▓ÓĖōÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣üÓĖźÓĖ░Ó╣ĆÓĖźÓĖĘÓĖŁÓĖöÓĖŚÓĖĄÓ╣łÓ╣äÓĖ½ÓĖźÓ╣ĆÓĖ¦ÓĖĄÓĖóÓĖÖ Ó╣āÓĖÖÓĖŻÓ╣łÓĖ▓ÓĖćÓĖüÓĖ▓ÓĖó ÓĖøÓĖŻÓĖ░ÓĖ¬ÓĖ┤ÓĖŚÓĖśÓĖ┤ÓĖĀÓĖ▓ÓĖ×ÓĖéÓĖŁÓĖć right ventricle Ó╣üÓĖźÓĖ░ venous capacitance ÓĖøÓĖŻÓĖ┤ÓĖĪÓĖ▓ÓĖōÓĖÖÓĖ│Ó╣ēÓĖ▓ÓĖ½ÓĖŻÓĖĘÓĖŁÓ╣ĆÓĖźÓĖĘÓĖŁÓĖöÓ╣āÓĖÖÓĖ½ÓĖ▒ÓĖ¦Ó╣āÓĖł ÓĖŗÓĖĄÓĖüÓĖŗÓ╣ēÓĖ▓ÓĖó (Left Atrial Pressure, LAP) ÓĖŁÓĖ▓ÓĖłÓĖ¦ÓĖ▒ÓĖöÓ╣éÓĖöÓĖóÓĖüÓĖ▓ÓĖŻÓ╣āÓĖ¬Ó╣ł ÓĖ¬ÓĖ▓ÓĖó polyvinyl catheter Ó╣ĆÓĖéÓ╣ēÓĖ▓Ó╣äÓĖøÓ╣āÓĖÖ left atrium Ó╣éÓĖöÓĖóÓĖĢÓĖŻÓĖćÓĖŻÓĖ░ÓĖ½ÓĖ¦Ó╣łÓĖ▓ÓĖćÓĖüÓĖ▓ÓĖŻÓĖ£Ó╣łÓĖ▓ÓĖĢÓĖ▒ÓĖöÓĖ½ÓĖ▒ÓĖ¦Ó╣āÓĖłÓ╣üÓĖÜÓĖÜÓ╣ĆÓĖøÓĖ┤ÓĖö ÓĖ½ÓĖŻÓĖĘÓĖŁÓ╣éÓĖöÓĖóÓ╣āÓĖ¬Ó╣ł Swan-Ganz catheter ÓĖ£Ó╣łÓĖ▓ÓĖÖÓĖŚÓĖ▓ÓĖćÓ╣ĆÓĖ¬Ó╣ēÓĖÖÓ╣ĆÓĖźÓĖĘÓĖŁÓĖöÓĖöÓĖ│ÓĖ▓Ó╣āÓĖ½ÓĖŹÓ╣łÓ╣ĆÓĖéÓ╣ēÓĖ▓ÓĖ¬ÓĖ╣Ó╣ł pulmonary artery Ó╣üÓĖźÓĖ░ÓĖ¦ÓĖ▒ÓĖö Pulmonary Capillary
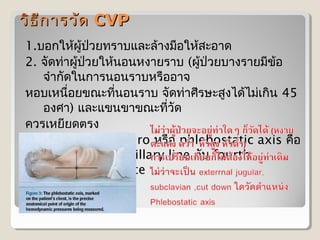
- 4. ÓĖ¦ÓĖ┤ÓĖś ÓĖü ÓĖ▓ÓĖŻÓĖ¦ÓĖ▒ÓĖö CVP ÓĖĄ 1.ÓĖÜÓĖŁÓĖüÓ╣āÓĖ½Ó╣ēÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖóÓĖŚÓĖŻÓĖ▓ÓĖÜÓ╣üÓĖźÓĖ░ÓĖźÓ╣ēÓĖ▓ÓĖćÓĖĪÓĖĘÓĖŁÓ╣āÓĖ½Ó╣ēÓĖ¬ÓĖ░ÓĖŁÓĖ▓ÓĖö 2. ÓĖłÓĖ▒ÓĖöÓĖŚÓ╣łÓĖ▓ÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖóÓ╣āÓĖ½Ó╣ēÓĖÖÓĖŁÓĖÖÓĖ½ÓĖćÓĖ▓ÓĖóÓĖŻÓĖ▓ÓĖÜ (ÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖóÓĖÜÓĖ▓ÓĖćÓĖŻÓĖ▓ÓĖóÓĖĪÓĖĄÓĖéÓ╣ēÓĖŁ ÓĖłÓĖ│ÓĖ▓ÓĖüÓĖ▒ÓĖöÓ╣āÓĖÖÓĖüÓĖ▓ÓĖŻÓĖÖÓĖŁÓĖÖÓĖŻÓĖ▓ÓĖÜÓĖ½ÓĖŻÓĖĘÓĖŁÓĖŁÓĖ▓ÓĖł ÓĖ½ÓĖŁÓĖÜÓ╣ĆÓĖ½ÓĖÖÓĖĘÓ╣łÓĖŁÓĖóÓĖéÓĖōÓĖ░ÓĖŚÓĖĄÓ╣łÓĖÖÓĖŁÓĖÖÓĖŻÓĖ▓ÓĖÜ ÓĖłÓĖ▒ÓĖöÓĖŚÓ╣łÓĖ▓ÓĖ©ÓĖĄÓĖŻÓĖ®ÓĖ░ÓĖ¬ÓĖ╣ÓĖćÓ╣äÓĖöÓ╣ēÓ╣äÓĖĪÓ╣łÓ╣ĆÓĖüÓĖ┤ÓĖÖ 45 ÓĖŁÓĖćÓĖ©ÓĖ▓) Ó╣üÓĖźÓĖ░Ó╣üÓĖéÓĖÖÓĖéÓĖ▓ÓĖéÓĖōÓĖ░ÓĖŚÓĖĄÓĖ¦ÓĖ▒ÓĖö Ó╣ł ÓĖäÓĖ¦ÓĖŻÓ╣ĆÓĖ½ÓĖóÓĖĄÓĖóÓĖöÓĖĢÓĖŻÓĖć 3. ÓĖ½ÓĖ▓ÓĖĢÓĖ│ÓĖ▓Ó╣üÓĖ½ÓĖÖÓ╣łÓĖćÓĖéÓĖŁÓĖć zero ÓĖ½ÓĖŻÓĖĘÓĖŁ phlebostatic axis ÓĖäÓĖĘÓĖŁ ÓĖłÓĖĖÓĖöÓĖĢÓĖ▒ÓĖöÓĖéÓĖŁÓĖć midaxillary line ÓĖüÓĖ▒ÓĖÜ fourth intercostal space
- 5. ÓĖ¦ÓĖ┤ÓĖś ÓĖü ÓĖ▓ÓĖŻÓĖ¦ÓĖ▒ÓĖö CVP ÓĖĄ
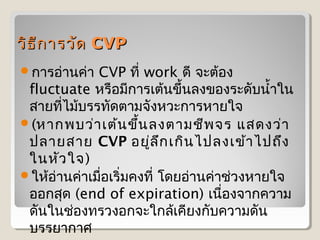
- 6. ÓĖ¦ÓĖ┤ÓĖś ÓĖĄÓĖü ÓĖ▓ÓĖŻÓĖ¦ÓĖ▒ÓĖö CVP ’éŚÓĖüÓĖ▓ÓĖŻÓĖŁÓ╣łÓĖ▓ÓĖÖÓĖäÓ╣łÓĖ▓ CVP ÓĖŚÓĖĄÓ╣ł work ÓĖöÓĖĄ ÓĖłÓĖ░ÓĖĢÓ╣ēÓĖŁÓĖć fluctuate ÓĖ½ÓĖŻÓĖĘÓĖŁÓĖĪÓĖĄÓĖüÓĖ▓ÓĖŻÓ╣ĆÓĖĢÓ╣ēÓĖÖÓĖéÓĖČÓ╣ēÓĖÖÓĖźÓĖćÓĖéÓĖŁÓĖćÓĖŻÓĖ░ÓĖöÓĖ▒ÓĖÜÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣āÓĖÖ ÓĖ¬ÓĖ▓ÓĖóÓĖŚÓĖĄÓ╣łÓ╣äÓĖĪÓ╣ēÓĖÜÓĖŻÓĖŻÓĖŚÓĖ▒ÓĖöÓĖĢÓĖ▓ÓĖĪÓĖłÓĖ▒ÓĖćÓĖ½ÓĖ¦ÓĖ░ÓĖüÓĖ▓ÓĖŻÓĖ½ÓĖ▓ÓĖóÓ╣āÓĖł ’éŚ(ÓĖ½ÓĖ▓ÓĖüÓĖ×ÓĖÜÓĖ¦Ó╣łÓĖ▓ Ó╣ĆÓĖĢÓ╣ēÓĖÖ ÓĖéÓĖČÓ╣ēÓĖÖ ÓĖźÓĖćÓĖĢÓĖ▓ÓĖĪÓĖŖÓĖĄÓĖ× ÓĖłÓĖŻ Ó╣üÓĖ¬ÓĖöÓĖćÓĖ¦Ó╣łÓĖ▓ ÓĖøÓĖźÓĖ▓ÓĖóÓĖ¬ÓĖ▓ÓĖó CVP ÓĖŁÓĖóÓĖ╣Ó╣łÓĖź ÓĖČÓĖü Ó╣ĆÓĖüÓĖ┤ÓĖÖ Ó╣äÓĖøÓĖźÓĖćÓ╣ĆÓĖéÓ╣ēÓĖ▓ Ó╣äÓĖøÓĖ¢ÓĖČÓĖć Ó╣āÓĖÖÓĖ½ÓĖ▒ÓĖ¦ Ó╣āÓĖł) ’éŚÓ╣āÓĖ½Ó╣ēÓĖŁÓ╣łÓĖ▓ÓĖÖÓĖäÓ╣łÓĖ▓Ó╣ĆÓĖĪÓĖĘÓ╣łÓĖŁÓ╣ĆÓĖŻÓĖ┤Ó╣łÓĖĪÓĖäÓĖćÓĖŚÓĖĄÓ╣ł Ó╣éÓĖöÓĖóÓĖŁÓ╣łÓĖ▓ÓĖÖÓĖäÓ╣łÓĖ▓ÓĖŖÓ╣łÓĖ¦ÓĖćÓĖ½ÓĖ▓ÓĖóÓ╣āÓĖł ÓĖŁÓĖŁÓĖüÓĖ¬ÓĖĖÓĖö (end of expiration) Ó╣ĆÓĖÖÓĖĘÓ╣łÓĖŁÓĖćÓĖłÓĖ▓ÓĖüÓĖäÓĖ¦ÓĖ▓ÓĖĪ ÓĖöÓĖ▒ÓĖÖÓ╣āÓĖÖÓĖŖÓ╣łÓĖŁÓĖćÓĖŚÓĖŻÓĖ¦ÓĖćÓĖŁÓĖüÓĖłÓĖ░Ó╣āÓĖüÓĖźÓ╣ēÓ╣ĆÓĖäÓĖĄÓĖóÓĖćÓĖüÓĖ▒ÓĖÜÓĖäÓĖ¦ÓĖ▓ÓĖĪÓĖöÓĖ▒ÓĖÖ ÓĖÜÓĖŻÓĖŻÓĖóÓĖ▓ÓĖüÓĖ▓ÓĖ©
- 7. ÓĖüÓĖ▓ÓĖŻÓ╣üÓĖøÓĖźÓĖäÓ╣łÓĖ▓ CVP ÓĖäÓ╣łÓĖ▓ CVP ÓĖøÓĖüÓĖĢÓĖ┤ ÓĖŁÓĖ▓ÓĖłÓĖŁÓĖóÓĖ╣Ó╣łÓ╣āÓĖÖÓĖŖÓ╣łÓĖ¦ÓĖć 6-12 cmH2O ÓĖŚÓĖ▒ÓĖćÓĖÖÓĖĄÓ╣ēÓĖĪÓĖü Ó╣ē ÓĖ▒ Ó╣āÓĖŖÓ╣ēÓĖäÓ╣łÓĖ▓ CVP Ó╣āÓĖÖÓĖüÓĖ▓ÓĖŻÓ╣ĆÓĖøÓĖŻÓĖĄÓĖóÓĖÜÓ╣ĆÓĖŚÓĖĄÓĖóÓĖÜÓĖüÓĖ▓ÓĖŻÓ╣ĆÓĖøÓĖźÓĖĄÓ╣łÓĖóÓĖÖÓ╣üÓĖøÓĖźÓĖćÓĖłÓĖ▓ÓĖü ÓĖüÓĖ▓ÓĖŻÓĖŻÓĖ▒ÓĖüÓĖ®ÓĖ▓Ó╣āÓĖÖÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖóÓĖŻÓĖ▓ÓĖóÓĖÖÓĖ▒ÓĖÖÓ╣å ÓĖĪÓĖ▓ÓĖüÓĖüÓĖ¦Ó╣łÓĖ▓ Ó╣ē ’éŚÓĖäÓ╣łÓĖ▓ CVP ÓĖĢÓĖ│Ó╣łÓĖ▓ ÓĖ½ÓĖĪÓĖ▓ÓĖóÓĖ¢ÓĖČÓĖć ÓĖøÓĖŻÓĖ┤ÓĖĪÓĖ▓ÓĖōÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣üÓĖźÓĖ░Ó╣ĆÓĖźÓĖĘÓĖŁÓĖöÓ╣āÓĖÖÓĖŻÓ╣łÓĖ▓ÓĖćÓĖüÓĖ▓ÓĖó ÓĖźÓĖöÓĖźÓĖć ’éŚÓĖäÓ╣łÓĖ▓ CVP ÓĖ¬ÓĖ╣ÓĖćÓĖéÓĖČÓ╣ēÓĖÖÓĖĪÓĖ▒ÓĖü ÓĖ½ÓĖĪÓĖ▓ÓĖóÓĖ¢ÓĖČÓĖćÓĖøÓĖŻÓĖ┤ÓĖĪÓĖ▓ÓĖōÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣üÓĖźÓĖ░Ó╣ĆÓĖźÓĖĘÓĖŁÓĖöÓ╣āÓĖÖ ÓĖŻÓ╣łÓĖ▓ÓĖćÓĖüÓĖ▓ÓĖóÓĖĪÓĖ▓ÓĖüÓĖéÓĖČÓ╣ēÓĖÖ ÓĖŚÓĖĄÓĖ¬ÓĖ│ÓĖ▓ÓĖäÓĖ▒ÓĖŹÓ╣āÓĖÖÓĖüÓĖ▓ÓĖŻÓ╣üÓĖøÓĖźÓĖäÓ╣łÓĖ▓ CVP ÓĖłÓĖ░ÓĖĢÓ╣ēÓĖŁÓĖćÓĖöÓĖ╣ Ó╣ł ÓĖŁÓĖ▓ÓĖüÓĖ▓ÓĖŻÓ╣üÓĖźÓĖ░ÓĖŁÓĖ▓ÓĖüÓĖ▓ÓĖŻÓ╣üÓĖ¬ÓĖöÓĖćÓĖŁÓĖĘÓ╣łÓĖÖÓĖŻÓ╣łÓĖ¦ÓĖĪÓĖöÓ╣ēÓĖ¦ÓĖó Ó╣ĆÓĖŖÓ╣łÓĖÖ blood pressure, heart rate, urine output, urine specific gravity, intake/output, conscious, ÓĖ¤ÓĖ▒ÓĖćÓĖøÓĖŁÓĖöÓ╣äÓĖöÓ╣ēÓĖóÓĖ┤ÓĖÖÓ╣ĆÓĖ¬ÓĖĄÓĖóÓĖćÓĖ£ÓĖ┤ÓĖöÓĖøÓĖüÓĖĢÓĖ┤ ÓĖŁÓĖ▓ÓĖüÓĖ▓ÓĖŻÓĖ½ÓĖŁÓĖÜÓ╣ĆÓĖ½ÓĖÖÓĖĘÓ╣łÓĖŁÓĖó ÓĖäÓĖ¦ÓĖ▓ÓĖĪ ÓĖĢÓĖČÓĖćÓĖĢÓĖ▒ÓĖ¦ ÓĖäÓĖ¦ÓĖ▓ÓĖĪÓĖŁÓĖĖÓ╣łÓĖÖ Ó╣ĆÓĖóÓ╣ćÓĖÖ ÓĖŖÓĖĘÓ╣ēÓĖÖÓĖéÓĖŁÓĖćÓĖ£ÓĖ┤ÓĖ¦ÓĖ½ÓĖÖÓĖ▒ÓĖć Ó╣ĆÓĖøÓ╣ćÓĖÖÓĖĢÓ╣ēÓĖÖ
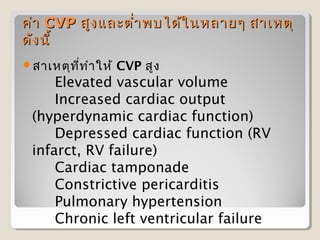
- 8. ÓĖäÓ╣łÓĖ▓ CVP ÓĖ¬ÓĖ╣ÓĖć Ó╣üÓĖźÓĖ░ÓĖĢÓĖ│Ó╣łÓĖ▓ ÓĖ×ÓĖÜÓ╣äÓĖöÓ╣ēÓ╣ā ÓĖÖÓĖ½ÓĖźÓĖ▓ÓĖóÓ╣å ÓĖ¬ÓĖ▓Ó╣ĆÓĖ½ÓĖĢÓĖĖ ÓĖöÓĖ▒ÓĖć ÓĖÖÓĖĄÓ╣ē ’éŚÓĖ¬ÓĖ▓Ó╣ĆÓĖ½ÓĖĢÓĖĖÓĖŚ ÓĖŚ ÓĖ│ÓĖ▓ Ó╣āÓĖ½Ó╣ē ÓĖĄÓ╣ł CVP ÓĖ¬ÓĖ╣ÓĖć Elevated vascular volume Increased cardiac output (hyperdynamic cardiac function) Depressed cardiac function (RV infarct, RV failure) Cardiac tamponade Constrictive pericarditis Pulmonary hypertension Chronic left ventricular failure
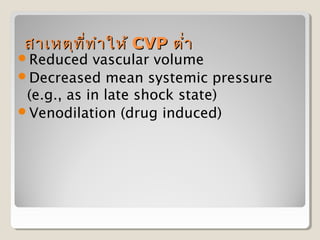
- 9. ÓĖ¬ÓĖ▓Ó╣ĆÓĖ½ÓĖĢÓĖĖÓĖŚ ÓĖĄÓ╣łÓĖŚ ÓĖ│ÓĖ▓ Ó╣āÓĖ½Ó╣ē CVP ÓĖĢÓĖ│Ó╣łÓĖ▓ ’éŚReduced vascular volume ’éŚDecreased mean systemic pressure (e.g., as in late shock state) ’éŚVenodilation (drug induced)
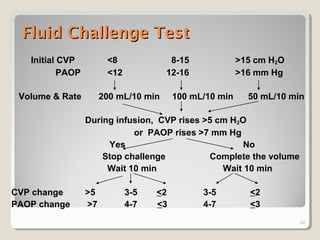
- 10. Fluid Challenge Test Initial CVP <8 8-15 >15 cm H2O PAOP <12 12-16 >16 mm Hg Volume & Rate 200 mL/10 min 100 mL/10 min 50 mL/10 min During infusion, CVP rises >5 cm H2O or PAOP rises >7 mm Hg Yes No Stop challenge Complete the volume Wait 10 min Wait 10 min CVP change >5 3-5 <2 3-5 <2 PAOP change >7 4-7 <3 4-7 <3 10
- 11. Central Venous Pressure Monitoring ’éŚÓĖéÓĖ▒Ó╣ēÓĖÖ ÓĖĢÓ╣łÓĖŁ ÓĖŁÓĖĖÓĖø ÓĖüÓĖŻÓĖōÓ╣ī ÓĖĢÓ╣łÓĖŁ set iv Ó╣ĆÓĖéÓ╣ēÓĖ▓ÓĖüÓĖ▒ÓĖÜ ÓĖéÓĖ¦ÓĖöÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣ĆÓĖüÓĖźÓĖĘÓĖŁ 0.9 NSS 100 ml. Ó╣üÓĖźÓ╣ēÓĖ¦ ÓĖĢÓ╣łÓĖŁÓĖ¬ÓĖ▓ÓĖó IV Ó╣ĆÓĖéÓ╣ēÓĖ▓ÓĖüÓĖ▒ÓĖÜÓĖĢÓĖ▒ÓĖ¦ transducer Ó╣üÓĖźÓ╣ēÓĖ¦ÓĖĢÓ╣łÓĖŁÓĖ¬ÓĖ▓ÓĖó extension Ó╣ĆÓĖéÓ╣ēÓĖ▓ÓĖüÓĖ▒ÓĖÜ transducer ÓĖĢÓ╣łÓĖŁÓ╣üÓĖøÓ╣ēÓĖÖ ÓĖ¬ÓĖ│ÓĖ▓ÓĖ½ÓĖŻÓĖ▒ÓĖÜÓĖ¦ÓĖ▓ÓĖćtransducerg Ó╣ĆÓĖéÓ╣ēÓĖ▓ÓĖüÓĖ▒ÓĖÜÓ╣ĆÓĖ¬ÓĖ▓ÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣ĆÓĖüÓĖźÓĖĘÓĖŁ Ó╣éÓĖöÓĖóÓĖĢÓĖ▒ÓĖ¦ Ó╣üÓĖøÓ╣ēÓĖÖÓĖĢÓ╣ēÓĖŁÓĖćÓĖŁÓĖóÓĖ╣Ó╣łÓ╣āÓĖÖÓĖĢÓĖ│ÓĖ▓Ó╣üÓĖ½ÓĖÖÓ╣łÓĖć phlebostatic axis ÓĖäÓĖĘÓĖŁ midaxillary line ÓĖüÓĖ▒ÓĖÜ fourth intercostal space
- 12. Central Venous Pressure Monitoring ’éŚÓĖłÓĖ▓ÓĖüÓĖÖÓĖ▒Ó╣ēÓĖÖÓ╣ĆÓĖøÓĖ┤ÓĖöÓĖÖÓĖ│Ó╣ēÓĖ▓Ó╣ĆÓĖüÓĖźÓĖĘÓĖŁ Ó╣ĆÓĖ×ÓĖĘÓ╣łÓĖŁÓ╣äÓĖźÓ╣ł air ÓĖŚÓĖĄÓ╣łÓĖŁÓĖóÓĖ╣Ó╣łÓ╣āÓĖÖ set ÓĖŚÓĖ▒Ó╣ēÓĖćÓĖ½ÓĖĪÓĖö Ó╣ĆÓĖ¬ÓĖŻÓ╣ćÓĖł Ó╣üÓĖźÓ╣ēÓĖ¦ÓĖĢÓ╣łÓĖŁÓĖ¬ÓĖ▓ÓĖó extension Ó╣ĆÓĖéÓ╣ēÓĖ▓ÓĖüÓĖ▒ÓĖÜ ÓĖ¬ÓĖ▓ÓĖó cutdown ÓĖ½ÓĖŻÓĖĘÓĖŁ subclavian vein Ó╣éÓĖöÓĖó subclavian ÓĖĢÓ╣łÓĖŁÓ╣ĆÓĖéÓ╣ēÓĖ▓ÓĖüÓĖ▒ÓĖÜÓĖ¬ÓĖ▓ÓĖó ÓĖ¬ÓĖĄ ÓĖÖÓĖ│Ó╣ēÓĖ▓ÓĖĢÓĖ▓ÓĖź ÓĖ½ÓĖŻÓĖĘÓĖŁ proximal lumen
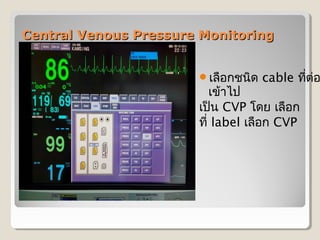
- 13. Central Venous Pressure Monitoring ’éŚÓĖĢÓ╣łÓĖŁmonitor ÓĖĢÓ╣łÓĖŁ ÓĖ¬ÓĖ▓ÓĖó cable Ó╣ĆÓĖéÓ╣ēÓĖ▓ÓĖŚÓĖĄÓ╣ł ÓĖłÓĖŁmonitor
- 14. Central Venous Pressure Monitoring ’éŚÓ╣ĆÓĖźÓĖĘÓĖŁÓĖüÓĖŖÓĖÖÓĖ┤ÓĖö cable ÓĖŚÓĖĄÓĖĢÓ╣łÓĖŁ Ó╣ł Ó╣ĆÓĖéÓ╣ēÓĖ▓Ó╣äÓĖø Ó╣ĆÓĖøÓ╣ćÓĖÖ CVP Ó╣éÓĖöÓĖó Ó╣ĆÓĖźÓĖĘÓĖŁÓĖü ÓĖŚÓĖĄÓ╣ł label Ó╣ĆÓĖźÓĖĘÓĖŁÓĖü CVP
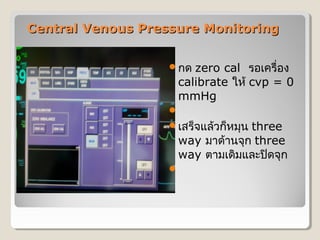
- 15. Central Venous Pressure Monitoring ’éŚÓĖüÓĖö zero cal ÓĖŻÓĖŁÓ╣ĆÓĖäÓĖŻÓĖĘÓ╣łÓĖŁÓĖć calibrate Ó╣āÓĖ½Ó╣ē cvp = 0 mmHg ’éŚ ’éŚÓ╣ĆÓĖ¬ÓĖŻÓ╣ćÓĖłÓ╣üÓĖźÓ╣ēÓĖ¦ÓĖüÓ╣ćÓĖ½ÓĖĪÓĖĖÓĖÖ three way ÓĖĪÓĖ▓ÓĖöÓ╣ēÓĖ▓ÓĖÖÓĖłÓĖĖÓĖü three way ÓĖĢÓĖ▓ÓĖĪÓ╣ĆÓĖöÓĖ┤ÓĖĪÓ╣üÓĖźÓĖ░ÓĖøÓĖ┤ÓĖöÓĖłÓĖĖÓĖü ’éŚ
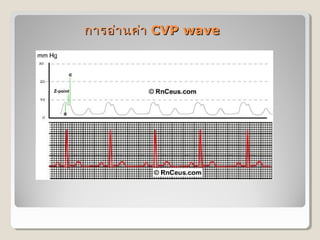
- 16. ÓĖüÓĖ▓ÓĖŻÓĖŁÓ╣łÓĖ▓ ÓĖÖÓĖäÓ╣łÓĖ▓ CVP wave
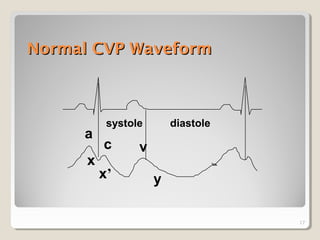
- 17. Normal CVP Waveform systole diastole a c v x xŌĆÖ y 17
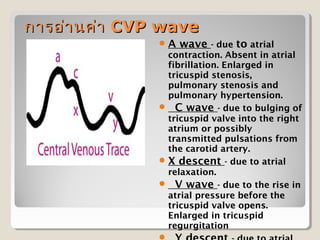
- 18. ÓĖüÓĖ▓ÓĖŻÓĖŁÓ╣łÓĖ▓ ÓĖÖÓĖäÓ╣łÓĖ▓ CVP wave ’éŚ A wave - due to atrial contraction. Absent in atrial fibrillation. Enlarged in tricuspid stenosis, pulmonary stenosis and pulmonary hypertension. ’éŚ ╠²C wave - due to bulging of tricuspid valve into the right atrium or possibly transmitted pulsations from the carotid artery. ’éŚ X descent - due to atrial relaxation. ’éŚ ╠²V wave - due to the rise in atrial pressure before the tricuspid valve opens. Enlarged in tricuspid regurgitation
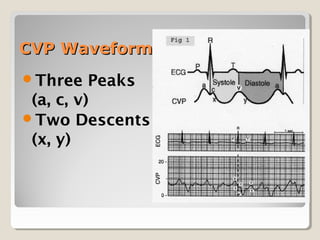
- 19. CVP Waveform ’éŚThree Peaks (a, c, v) ’éŚTwo Descents (x, y)
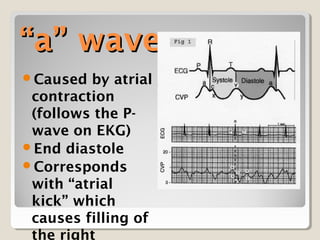
- 20. ŌĆ£aŌĆØ wave ’éŚCaused by atrial contraction (follows the P- wave on EKG) ’éŚEnd diastole ’éŚCorresponds with ŌĆ£atrial kickŌĆØ which causes filling of the right
- 21. ŌĆ£cŌĆØ wave ’éŚAtrial pressure decreases after the ŌĆ£aŌĆØ wave as a result of atrial relaxation ’éŚThe ŌĆ£cŌĆØ wave is due to isovolemic right ventricular contraction; closes the tricuspid valve and causes it to
- 22. ŌĆ£xŌĆØ descent ’éŚAtrial pressure continues to decline due to atrial relaxation and changes in geometry caused by ventricular contraction ’éŚMid-systolic event ’éŚŌĆ£Systolic collapse in atrial pressureŌĆØ
- 23. ŌĆ£vŌĆØ wave ’éŚThe last atrial pressure increase is caused by filling of the atrium with blood from the vena cava ’éŚOccurs in late systole with the tricuspid still closed
- 24. ŌĆ£yŌĆØ descent ’éŚDecrease in atrial pressure as the tricuspid opens and blood flows from atrium to ventricle ’éŚŌĆ£Diastolic collapse in atrial pressureŌĆØ
- 25. Tricuspid Regurgitation ’éŚThe right atrium gains volume during systole - so the ŌĆ£cŌĆØ and ŌĆ£vŌĆØ wave is much higher ’éŚThe right atrium ŌĆ£seesŌĆØ right ventricular pressures and the pressure
- 26. Tricuspid Stenosis ’éŚ Problem with atrial emptying and a barrier to ventricular filling on the right side of the heart ’éŚ Mean CVP is elevated ’éŚ ŌĆ£aŌĆØ wave is usually prominent as it tries to overcome the barrier to emptying ’éŚ ŌĆ£yŌĆØ descent muted as a result of decreased outflow from atrium to ventricle
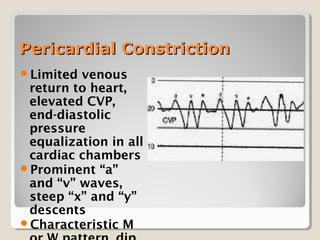
- 27. Pericardial Constriction ’éŚLimited venous return to heart, elevated CVP, end-diastolic pressure equalization in all cardiac chambers ’éŚProminent ŌĆ£aŌĆØ and ŌĆ£vŌĆØ waves, steep ŌĆ£xŌĆØ and ŌĆ£yŌĆØ descents ’éŚCharacteristic M
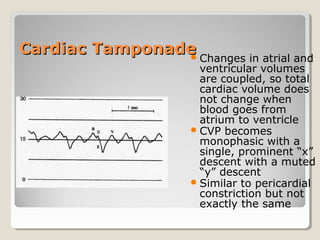
- 28. Cardiac Tamponade ’éŚ Changes in atrial and ventricular volumes are coupled, so total cardiac volume does not change when blood goes from atrium to ventricle ’éŚ CVP becomes monophasic with a single, prominent ŌĆ£xŌĆØ descent with a muted ŌĆ£yŌĆØ descent ’éŚ Similar to pericardial constriction but not exactly the same
- 29. ÓĖĀÓĖ▓ÓĖ¦ÓĖ░Ó╣üÓĖŚÓĖŻÓĖüÓĖŗÓ╣ēÓĖŁ ÓĖÖÓĖŚÓĖ▒Ó╣ēÓĖć ÓĖłÓĖ▓ÓĖüÓĖéÓĖ▒Ó╣ēÓĖÖ ÓĖĢÓĖŁÓĖÖÓĖüÓĖ▓ÓĖŻÓ╣āÓĖ¬Ó╣łÓĖ¬ ÓĖ▓ÓĖó CVP Ó╣üÓĖźÓĖ░ÓĖüÓĖ▓ÓĖŻÓĖ¦ÓĖ▒ÓĖö ÓĖĪÓĖĄÓĖö ÓĖ▒ÓĖć ÓĖÖÓĖĄÓ╣ē ’éŚ 1.╠² Hemothorax ’éŚ 2.╠² Pneumothorax ’éŚ 3.╠² Nerve injury ’éŚ 4.╠² Arterial puncture ’éŚ 5.╠² Thoracic duct perforation ’éŚ 6.╠² Arrhythmias ’éŚ 7.╠² Systemic or local infection ’éŚ 8.╠² Perforation or erosion of vascular structure ’éŚ 9.╠² Thrombosis ’éŚ 10.╠²╠²Air embolism ’éŚ 11.╠²╠²Blood loss ÓĖłÓĖ▓ÓĖüÓĖéÓ╣ēÓĖŁ ÓĖĢÓ╣łÓĖŁ ÓĖ½ÓĖźÓĖĖÓĖö ’éŚ 12.╠²╠²Volume overload ÓĖłÓĖ▓ÓĖüÓĖźÓĖĘÓĖĪ ÓĖøÓĖŻÓĖ▒ÓĖÜ rate IV ÓĖ½ÓĖźÓĖ▒ÓĖć ÓĖ¦ÓĖ▒ÓĖö CVP╠²╠²
Editor's Notes
- #6: ÓĖ½ÓĖĪÓĖĖÓĖÖ three-way Ó╣āÓĖ½Ó╣ē IV fluid Ó╣äÓĖ½ÓĖźÓ╣ĆÓĖéÓ╣ēÓĖ▓Ó╣äÓĖøÓ╣āÓĖÖÓĖ¬ÓĖ▓ÓĖó iv ÓĖöÓ╣ēÓĖ▓ÓĖÖÓ╣äÓĖĪÓ╣ēÓĖÜÓĖŻÓĖŻÓĖŚÓĖ▒ÓĖö Ó╣éÓĖöÓĖóÓĖøÓĖ┤ÓĖöÓĖöÓ╣ēÓĖ▓ÓĖÖÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖóÓ╣äÓĖ¦Ó╣ēÓĖüÓ╣łÓĖŁÓĖÖ ÓĖäÓĖ¦ÓĖŻÓ╣āÓĖ½Ó╣ē IV fluid ÓĖŁÓĖóÓĖ╣Ó╣łÓ╣āÓĖÖÓĖ¬ÓĖ▓ÓĖó Ó╣āÓĖÖÓĖŻÓĖ░ÓĖöÓĖ▒ÓĖÜÓ╣ĆÓĖüÓĖĘÓĖŁÓĖÜÓ╣ĆÓĖĢÓ╣ćÓĖĪÓĖ¬ÓĖ▓ÓĖó ÓĖ½ÓĖŻÓĖĘÓĖŁÓĖĪÓĖ▓ÓĖüÓĖüÓĖ¦Ó╣łÓĖ▓ÓĖäÓ╣łÓĖ▓Ó╣ĆÓĖöÓĖ┤ÓĖĪ ( ÓĖøÓĖŻÓĖ░ÓĖĪÓĖ▓ÓĖō 5 cm) ÓĖłÓĖ▓ÓĖüÓĖÖÓĖ▒Ó╣ēÓĖÖÓĖ½ÓĖĪÓĖĖÓĖÖÓĖøÓĖ┤ÓĖö three-way ÓĖöÓ╣ēÓĖ▓ÓĖÖÓ╣äÓĖĪÓ╣ēÓĖÜÓĖŻÓĖŻÓĖŚÓĖ▒ÓĖö 5. ÓĖÖÓĖ│Ó╣äÓĖĪÓ╣ēÓĖÜÓĖŻÓĖŻÓĖŚÓĖ▒ÓĖöÓĖ¦ÓĖ▓ÓĖćÓĖŚÓĖ▓ÓĖÜÓĖŚÓĖĄÓ╣łÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖó Ó╣éÓĖöÓĖóÓ╣āÓĖ½Ó╣ēÓĖĢÓĖ│Ó╣üÓĖ½ÓĖÖÓ╣łÓĖćÓĖéÓĖŁÓĖć zero ÓĖ½ÓĖŻÓĖĘÓĖŁÓ╣ĆÓĖźÓĖéÓĖ©ÓĖ╣ÓĖÖÓĖóÓ╣ī ÓĖŗÓĖČÓ╣łÓĖćÓĖłÓĖĖÓĖöÓĖŚÓĖĄÓ╣łÓĖ¦ÓĖ▓ÓĖćÓĖĢÓ╣ēÓĖŁÓĖćÓĖŁÓĖóÓĖ╣Ó╣łÓĖŻÓĖ░ÓĖöÓĖ▒ÓĖÜÓ╣ĆÓĖöÓĖĄÓĖóÓĖ¦ÓĖüÓĖ▒ÓĖÜ right atrium ÓĖÖÓĖ▒Ó╣łÓĖÖÓĖäÓĖĘÓĖŁÓĖŚÓĖĄÓ╣łÓĖĢÓĖ│Ó╣üÓĖ½ÓĖÖÓ╣łÓĖćÓĖłÓĖĖÓĖöÓĖĢÓĖ▒ÓĖöÓĖéÓĖŁÓĖć midaxillary line ÓĖüÓĖ▒ÓĖÜ fourth intercostal space 6. ÓĖ½ÓĖĪÓĖĖÓĖÖ three-way Ó╣ĆÓĖøÓĖ┤ÓĖöÓ╣ĆÓĖēÓĖ×ÓĖ▓ÓĖ░ÓĖöÓ╣ēÓĖ▓ÓĖÖÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖóÓĖüÓĖ▒ÓĖÜÓ╣äÓĖĪÓ╣ēÓĖÜÓĖŻÓĖŻÓĖŚÓĖ▒ÓĖö ÓĖøÓĖ┤ÓĖöÓĖöÓ╣ēÓĖ▓ÓĖÖ IV ( ÓĖüÓĖŻÓĖōÓĖĄÓĖŚÓĖĄÓ╣łÓĖĪÓĖĄ three-way ÓĖ½ÓĖźÓĖ▓ÓĖóÓĖŁÓĖ▒ÓĖÖ Ó╣āÓĖ½Ó╣ēÓĖøÓĖŻÓĖ▒ÓĖÜÓ╣ĆÓĖēÓĖ×ÓĖ▓ÓĖ░ÓĖŁÓĖ▒ÓĖÖÓĖŚÓĖĄÓ╣łÓĖŁÓĖóÓĖ╣Ó╣łÓĖĢÓĖ┤ÓĖöÓĖüÓĖ▒ÓĖÜÓĖ¬ÓĖ▓ÓĖó cut down ÓĖ½ÓĖŻÓĖĘÓĖŁÓĖŁÓĖ▒ÓĖÖÓĖŚÓĖĄÓ╣łÓĖĪÓĖĄÓ╣äÓĖĪÓ╣ēÓĖÜÓĖŻÓĖŻÓĖŚÓĖ▒ÓĖö )
- #11: ÓĖ¢Ó╣ēÓĖ▓ÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖóÓĖĪÓĖĄÓĖäÓ╣łÓĖ▓ CVP ÓĖ¬ÓĖ╣ÓĖćÓ╣üÓĖĢÓ╣łÓĖĪÓĖĄÓĖŁÓĖ▓ÓĖüÓĖ▓ÓĖŻ Ó╣äÓĖĪÓ╣łÓĖ¬ÓĖŁÓĖöÓĖäÓĖźÓ╣ēÓĖŁÓĖćÓĖüÓĖ▒ÓĖÜÓĖäÓ╣łÓĖ▓ CVP ÓĖäÓĖĘÓĖŁ HR Ó╣ĆÓĖŻÓ╣ćÓĖ¦ ÓĖŗÓĖČÓ╣łÓĖćÓĖäÓ╣łÓĖ▓ CVP ÓĖŚÓĖĄÓ╣łÓĖ¬ÓĖ╣ÓĖćÓĖŁÓĖ▓ÓĖłÓ╣ĆÓĖüÓĖ┤ÓĖöÓĖłÓĖ▓ÓĖüÓĖäÓĖ¦ÓĖ▓ÓĖĪÓĖöÓĖ▒ÓĖÖÓ╣āÓĖÖÓĖŖÓ╣łÓĖŁÓĖćÓĖŁÓĖŁÓĖüÓĖ¬ÓĖ╣ÓĖć Ó╣ĆÓĖŖÓ╣łÓĖÖ high PEEP Ó╣āÓĖ½Ó╣ēÓĖŚÓĖ│ÓĖüÓĖ▓ÓĖŻ challenge test
- #16: ÓĖ¢ÓĖČÓĖćÓĖéÓĖ▒Ó╣ēÓĖÖÓĖĢÓĖŁÓĖÖ calibration Ó╣ĆÓĖĪÓĖĘÓ╣łÓĖŁÓĖ¦ÓĖ▓ÓĖćÓĖĢÓĖ│Ó╣üÓĖ½ÓĖÖÓ╣łÓĖć transcuder ÓĖŚÓĖĄÓ╣łÓĖłÓĖĖÓĖö phlebostatic axis Ó╣üÓĖźÓ╣ēÓĖ¦ ÓĖ½ÓĖĪÓĖĖÓĖÖ three way ÓĖéÓĖŁÓĖć transducer ÓĖöÓ╣ēÓĖ▓ÓĖÖÓĖ£ÓĖ╣Ó╣ēÓĖøÓ╣łÓĖ¦ÓĖó Ó╣üÓĖźÓ╣ēÓĖ¦Ó╣ĆÓĖøÓĖ┤ÓĖöÓĖłÓĖĖÓĖü ÓĖŁÓĖŁÓĖü ŌĆ£ close patient open to airŌĆØ ÓĖ½ÓĖĪÓĖ▓ÓĖóÓ╣ĆÓĖ½ÓĖĢÓĖĖ ÓĖäÓĖ¦ÓĖŻÓĖŚÓĖ│ÓĖüÓĖ▓ÓĖŻ flush ÓĖ¬ÓĖ▓ÓĖó CVP ÓĖŚÓĖĖÓĖüÓ╣ĆÓĖ¦ÓĖŻ Ó╣ĆÓĖ×ÓĖĘÓ╣łÓĖŁÓĖøÓ╣ēÓĖŁÓĖćÓĖüÓĖ▒ÓĖÖÓĖüÓĖ▓ÓĖŻÓĖŁÓĖĖÓĖöÓĖĢÓĖ▒ÓĖÖÓĖéÓĖŁÓĖćÓĖ¬ÓĖ▓ÓĖó Ó╣üÓĖźÓĖ░ cribrate Ó╣ĆÓĖĪÓĖĘÓ╣łÓĖŁ wave CVP Ó╣ĆÓĖĪÓĖĘÓ╣łÓĖŁÓĖĪÓĖĄÓĖüÓĖ▓ÓĖŻ Overdamping ╠²