Procalcitonin
•Download as DOCX, PDF•
6 likes•3,246 views
Chỉ điểm tình trạng nhiễm khuẩn
1 of 2
Downloaded 42 times

Recommended
CHẨN ĐOÁN VÀ ĐIỀU TRỊ NHIỄM TRÙNG HUYẾT SỐC NHIỄM TRÙNG



CHẨN ĐOÁN VÀ ĐIỀU TRỊ NHIỄM TRÙNG HUYẾT SỐC NHIỄM TRÙNGSoM
Ã˝
CH·∫®N ƒêO√ÅN V√Ä ƒêI·ªÄU TR·ªä NHI·ªÑM TR√ôNG HUY·∫æT S·ªêC NHI·ªÑM TR√ôNGTi·∫øp c·∫≠n ≤˙·ªán≥Û nh√¢n toan chuy·ªÉn h√≥a



Ti·∫øp c·∫≠n ≤˙·ªán≥Û nh√¢n toan chuy·ªÉn h√≥along le xuan
Ã˝
Toan chuy·ªÉn h√≥a l√† m·ªôt kh√°i ni·ªám r·∫•t th∆∞·ªùng g·∫∑p trong th·ª©c h√†nh l√¢m s√†ng, ƒë·∫∑c bi·ªát c√°c khoa ICU, c·∫•p c·ª©u, n·ªôi ti·∫øt...c√°ch ti·∫øp c·∫≠n khoa h·ªçc v√† hi·ªÉu r√µ c∆° ch·∫ø g·∫ßn nh∆∞ l√† x∆∞∆°ng s·ªëng c·ªßa vi·ªác ƒë√°nh gi√° m·ªôt ≤˙·ªán≥Û nh√¢n trong t√¨nh tr·∫°ng toan chuy·ªÉn h√≥a. Toan h√≥a m√°u kh√¥ng kh√≥ ƒë·ªÉ nh·∫≠n di·ªán nh∆∞ng nh·∫≠n di·ªán th·∫ø n√†o cho ƒë√∫ng l·∫°i l√† m·ªôt v·∫•n ƒë·ªÅ kh√°c.ho ra mau chan doan nguyen nhan va dieu tri



ho ra mau chan doan nguyen nhan va dieu triLuanvanyhoc.com-Zalo 0927.007.596
Ã˝
Ho ra máu chẩn đoán nguyên nhân và điều trị
Bs Nguyễn Quang Hòa
Ho ra máu được định nghĩa là ho khạc ra máu có nguồn
gốc từ đường hô hấp dưới.
• Là triệu chứng nặng có thể đe dọa đến tính mạng của
≤˙·ªán≥Û l√Ω l·ªìng ng·ª±c v√† c·∫ßn ph·∫£i c√≥ c√°c thƒÉm d√≤ c·∫•p.
Phổi được cấp máu bởi 2 hệ thống động mạch, bao gồm:
– (a) Động mạch phổi, cung cấp khoảng 99% máu động mạch cho
phổi và tham gia vào quá trình trao đổi khí.
– (b) Động mạch phế quản, là động mạch nuôi dưỡng các cấu trúc của đường hô hấp và các động mạch phổi (vasa vasorum),không tham gia vào quá trình trao đổi khí và nối thông với hệ mao mạch phổi.Dat catheter-tinh-mach-trung-tam



Dat catheter-tinh-mach-trung-tambanbientap
Ã˝
Đặt catheter tĩnh mạch trung tâm - BS Văn Đức Hạnh - Viện Tim mạch Việt NamCập nhật về điều trị nhiễm khuẩn huyết nặng và sốc nhiễm khuẩn-11-2015



Cập nhật về điều trị nhiễm khuẩn huyết nặng và sốc nhiễm khuẩn-11-2015SỨC KHỎE VÀ CUỘC SỐNG
Ã˝
BS Đỗ Quốc Huy, BV Nhân Dân 115Biến chứng cấp tính của Đái tháo đường



Biến chứng cấp tính của Đái tháo đườngSỨC KHỎE VÀ CUỘC SỐNG
Ã˝
Trần Thị Thùy DungDiagnostic_Dossier_December_2014_HE



Diagnostic_Dossier_December_2014_HEDr.Sutirtha Chakraborty,MD,FACB
Ã˝
Sepsis is a life-threatening condition caused by the body's response to an infection. It is difficult to diagnose but prompt treatment is important to prevent serious complications like organ failure and death. Procalcitonin (PCT) is a biomarker that has been shown to help diagnose sepsis and guide antibiotic treatment decisions. PCT levels rise more significantly in response to bacterial infections compared to other conditions. Several studies have found that using PCT levels to guide antibiotic therapy can reduce antibiotic use without worsening outcomes for patients with sepsis. While PCT is not a perfect diagnostic tool, it provides useful information when interpreted together with a patient's full clinical picture.The role of human factors in the fight against sepsis



The role of human factors in the fight against sepsisGiulio Toccafondi
Ã˝
the human factors approach can trasform the sepsis challenges into opportunities for improving the health care systemMore Related Content
What's hot (20)
ho ra mau chan doan nguyen nhan va dieu tri



ho ra mau chan doan nguyen nhan va dieu triLuanvanyhoc.com-Zalo 0927.007.596
Ã˝
Ho ra máu chẩn đoán nguyên nhân và điều trị
Bs Nguyễn Quang Hòa
Ho ra máu được định nghĩa là ho khạc ra máu có nguồn
gốc từ đường hô hấp dưới.
• Là triệu chứng nặng có thể đe dọa đến tính mạng của
≤˙·ªán≥Û l√Ω l·ªìng ng·ª±c v√† c·∫ßn ph·∫£i c√≥ c√°c thƒÉm d√≤ c·∫•p.
Phổi được cấp máu bởi 2 hệ thống động mạch, bao gồm:
– (a) Động mạch phổi, cung cấp khoảng 99% máu động mạch cho
phổi và tham gia vào quá trình trao đổi khí.
– (b) Động mạch phế quản, là động mạch nuôi dưỡng các cấu trúc của đường hô hấp và các động mạch phổi (vasa vasorum),không tham gia vào quá trình trao đổi khí và nối thông với hệ mao mạch phổi.Dat catheter-tinh-mach-trung-tam



Dat catheter-tinh-mach-trung-tambanbientap
Ã˝
Đặt catheter tĩnh mạch trung tâm - BS Văn Đức Hạnh - Viện Tim mạch Việt NamCập nhật về điều trị nhiễm khuẩn huyết nặng và sốc nhiễm khuẩn-11-2015



Cập nhật về điều trị nhiễm khuẩn huyết nặng và sốc nhiễm khuẩn-11-2015SỨC KHỎE VÀ CUỘC SỐNG
Ã˝
BS Đỗ Quốc Huy, BV Nhân Dân 115Biến chứng cấp tính của Đái tháo đường



Biến chứng cấp tính của Đái tháo đườngSỨC KHỎE VÀ CUỘC SỐNG
Ã˝
Trần Thị Thùy DungCập nhật về điều trị nhiễm khuẩn huyết nặng và sốc nhiễm khuẩn-11-2015



Cập nhật về điều trị nhiễm khuẩn huyết nặng và sốc nhiễm khuẩn-11-2015SỨC KHỎE VÀ CUỘC SỐNG
Ã˝
Viewers also liked (13)
Diagnostic_Dossier_December_2014_HE



Diagnostic_Dossier_December_2014_HEDr.Sutirtha Chakraborty,MD,FACB
Ã˝
Sepsis is a life-threatening condition caused by the body's response to an infection. It is difficult to diagnose but prompt treatment is important to prevent serious complications like organ failure and death. Procalcitonin (PCT) is a biomarker that has been shown to help diagnose sepsis and guide antibiotic treatment decisions. PCT levels rise more significantly in response to bacterial infections compared to other conditions. Several studies have found that using PCT levels to guide antibiotic therapy can reduce antibiotic use without worsening outcomes for patients with sepsis. While PCT is not a perfect diagnostic tool, it provides useful information when interpreted together with a patient's full clinical picture.The role of human factors in the fight against sepsis



The role of human factors in the fight against sepsisGiulio Toccafondi
Ã˝
the human factors approach can trasform the sepsis challenges into opportunities for improving the health care system194504028 cc8872



194504028 cc8872homeworkping3
Ã˝
homework help,online homework help,online tutors,online tutoring,research paper help,do my homework,
https://www.homeworkping.com/The third international consensus definitions for sepsis and septic shock (se...



The third international consensus definitions for sepsis and septic shock (se...Daniela Botero Echeverri
Ã˝
The document summarizes the process undertaken by an international task force to update the definitions of sepsis and septic shock based on advances in understanding of the pathobiology of sepsis since the prior definitions from 2001. The task force developed new definitions of sepsis as a life-threatening organ dysfunction caused by a dysregulated host response to infection, and of septic shock as a subset of sepsis with profound circulatory and metabolic abnormalities. Clinical criteria including changes in SOFA scores and vasopressor requirements were recommended to operationalize the new definitions in practice.Procalcitonin and MR-proAdrenomedullin as diagnostic and prognostic biomarker...



Procalcitonin and MR-proAdrenomedullin as diagnostic and prognostic biomarker...Vall d'Hebron Institute of Research (VHIR)
Ã˝
Andrea Senna's predoctoral presentation at 6th VHIR Scientific Session. Watch the video of the presentation after the last slide.ACTEP2014: Sepsis marker in clinical use



ACTEP2014: Sepsis marker in clinical usetaem
Ã˝
This document discusses sepsis markers and their clinical use. It summarizes several biomarkers that show potential for diagnosing and monitoring sepsis, including procalcitonin (PCT), C-reactive protein (CRP), and soluble CD14 subtype (sCD14-ST). sCD14-ST shows diagnostic value in distinguishing infection from SIRS and sepsis from severe sepsis. Studies found sCD14-ST levels correlated with severity of illness and organ dysfunction in sepsis patients. The document reviews several clinical trials and studies that evaluated these biomarkers for diagnosing and predicting outcomes in sepsis, abdominal infections, febrile neutropenia, and burns.

Significance of serum procalcitonin in sepsis



Significance of serum procalcitonin in sepsisLakshya K Solanki
Ã˝
The document discusses a study on sepsis in Indian patients admitted to the ICU. It finds that respiratory infections were the most common cause of sepsis. The study evaluated procalcitonin (PCT) levels to diagnose sepsis and found it to have 94% sensitivity. Higher PCT levels correlated with increased organ dysfunction as measured by SOFA scores. The study concludes PCT is a promising marker for diagnosing sepsis in critically ill patients that can help guide early management.ƒê·∫∑c ƒëi·ªÉm l√¢m s√†ng, c·∫≠n l√¢m s√†ng v√† ƒëi·ªÅu tr·ªã vi√™m ph·ªïi c·ªông ƒë·ªìng ·ªü ≤˙·ªán≥Û nh√¢n n...



ƒê·∫∑c ƒëi·ªÉm l√¢m s√†ng, c·∫≠n l√¢m s√†ng v√† ƒëi·ªÅu tr·ªã vi√™m ph·ªïi c·ªông ƒë·ªìng ·ªü ≤˙·ªán≥Û nh√¢n n...Luanvanyhoc.com-Zalo 0927.007.596
Ã˝
ƒê·∫∑c ƒëi·ªÉm l√¢m s√†ng, c·∫≠n l√¢m s√†ng v√† ƒëi·ªÅu tr·ªã vi√™m ph·ªïi c·ªông ƒë·ªìng ·ªü ≤˙·ªán≥Û nh√¢n nghi·ªán r∆∞·ª£u v√†o c·∫•p c·ª©u t·∫°i ≤˙·ªán≥Û vi·ªán B·∫°ch Mai
Phí tải ,20.000đ liên hệ quangthuboss@gmail.com 0904.704.374Biomarkers in Emergency Medicine: Katrin Hruska



Biomarkers in Emergency Medicine: Katrin HruskaSMACC Conference
Ã˝
Katrin Hruska discusses the usefulness of biomarkers in Emergency Medicine.
All biomarkers are awesome predictors of badness. Elevated hS-troponins after non-cardiac surgery or an acute exacerbation of COPD are associated with increased mortality.
In seemingly healthy people, elevated D-dimer levels are associated with increased mortality. Similarly, NT-proBNP levels predict mortality in patients with end-stage renal disease.
A biomarker, in its broadest sense, is defined as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention” (NIH Biomarkers Definitions Working group, 2001).
This definition includes everything from laboratory tests to blood pressure measurements or an ultrasound scan. The clinical assessment in the Emergency Department is based on the subjective history of the patient and all available biomarkers (and their change over time).
If we assume that biomarkers are objectively measured, there is an overestimation of their individual importance.
As Katrin explains, over testing and over diagnosis have serious consequences. Not only for patients but also for the healthcare system.
In a clinical context the ease of getting a laboratory test leads to a lower threshold for testing. This increases testing without affecting relevant clinical endpoints. Also, when a biomarker becomes part of the standardised workup for a certain symptom, primary care centres and emergency telephone services will refer patients to the Emergency Department for testing, even when the pretest probability is low.
Katrin contends this bias is not an inherent problem of biomarkers themselves, but of the decision-making process of clinicians. The human brain fears uncertainty. Anything that adds to the feeling of knowing is rewarding, which is the most probable explanation of over testing in settings where medico-legal risks for the clinicians are low.
There is an ever-increasing number of patients seeking to rule out serious conditions by relying on biomarker testing to provide certainty.Các dung dịch thường dùng trong hscc yhocthuchanh2015



Các dung dịch thường dùng trong hscc yhocthuchanh2015Tuấn Anh Bùi
Ã˝
các dung dich và chế phẩmĐịnh nghĩa mới về Sepsis 3.0



Định nghĩa mới về Sepsis 3.0Thanh Liem Vo
Ã˝
định nghĩa mới về phạm trù nhiễm trùng huyếtThe third international consensus definitions for sepsis and septic shock (se...



The third international consensus definitions for sepsis and septic shock (se...Daniela Botero Echeverri
Ã˝
Procalcitonin and MR-proAdrenomedullin as diagnostic and prognostic biomarker...



Procalcitonin and MR-proAdrenomedullin as diagnostic and prognostic biomarker...Vall d'Hebron Institute of Research (VHIR)
Ã˝


ƒê·∫∑c ƒëi·ªÉm l√¢m s√†ng, c·∫≠n l√¢m s√†ng v√† ƒëi·ªÅu tr·ªã vi√™m ph·ªïi c·ªông ƒë·ªìng ·ªü ≤˙·ªán≥Û nh√¢n n...



ƒê·∫∑c ƒëi·ªÉm l√¢m s√†ng, c·∫≠n l√¢m s√†ng v√† ƒëi·ªÅu tr·ªã vi√™m ph·ªïi c·ªông ƒë·ªìng ·ªü ≤˙·ªán≥Û nh√¢n n...Luanvanyhoc.com-Zalo 0927.007.596
Ã˝
Similar to Procalcitonin (20)
giảm tiểu cầu miễn dịch ở trẻ em những điểm mới trong thực hành lâm sàng



giảm tiểu cầu miễn dịch ở trẻ em những điểm mới trong thực hành lâm sàngboo boo
Ã˝
gi·∫£m ti·ªÉu c·∫ßu mi·ªÖn d·ªãch ·ªü tr·∫ª em nh·ªØng ƒëi·ªÉm m·ªõi trong th·ª±c h√†nh l√¢m s√†ng1. C∆°n b√£o Cytokines ·ªü ≤˙·ªán≥Û nh√¢n Covid-19 - TS.Huy.pdf



1. C∆°n b√£o Cytokines ·ªü ≤˙·ªán≥Û nh√¢n Covid-19 - TS.Huy.pdfSoM
Ã˝
1. C∆°n b√£o Cytokines ·ªü ≤˙·ªán≥Û nh√¢n Covid-19 - TS.Huy.pdfTh√¥ng tin thu·ªëc th√°ng 8/2014 c·ªßa B·ªánh vi√™n ƒêa Kh√≥a ƒê√† N·∫µng



Thông tin thuốc tháng 8/2014 của Bệnh viên Đa Khóa Đà NẵngHA VO THI
Ã˝
Bản tin "Thông tin thuốc" tháng 8 năm 2014, tài liệu lưu hành nội bộ của Khoa Dược biên soạn, nhằm đến đối tượng là bác sĩ tại BV Đa khoa Đà NẵngHội chứng viêm



Hội chứng viêmThanh Liem Vo
Ã˝
Hội chứng viêm và các dấu chứng của phản ứng viêmvai trò của procalcitonin trong nhận định dấu hiệu nhiễm trùng và hướng dẫn s...



vai trò của procalcitonin trong nhận định dấu hiệu nhiễm trùng và hướng dẫn s...SoM
Ã˝
hồi sứcCác chiến lược phân loại và điều trị viêm phổi cộng đồng 2020.pdf



Các chiến lược phân loại và điều trị viêm phổi cộng đồng 2020.pdfleonidas2507
Ã˝
Các chiến lược phân loại và điều trị viêm phổi cộng đồng 2020Viêm phổi



Viêm phổiUpdate Y học
Ã˝
Tải ứng dụng để xem đầy đủ
https://teraapp.net/public/downloadapp?companyId=45725Nghiên cứu ngộ độc thuốc trừ sâu phopho hữu cơ 



Nghiên cứu ngộ độc thuốc trừ sâu phopho hữu cơ SoM
Ã˝
Nghiên cứu ngộ độc thuốc trừ sâu phopho hữu cơ Lựa chọn kháng sinh hợp lý trong viêm phổi cộng đồng .pptx



Lựa chọn kháng sinh hợp lý trong viêm phổi cộng đồng .pptxCong Duy
Ã˝
Viêm phổi côngh đồnggiảm tiểu cầu miễn dịch ở trẻ em những điểm mới trong thực hành lâm sàng



giảm tiểu cầu miễn dịch ở trẻ em những điểm mới trong thực hành lâm sàngboo boo
Ã˝
vai trò của procalcitonin trong nhận định dấu hiệu nhiễm trùng và hướng dẫn s...



vai trò của procalcitonin trong nhận định dấu hiệu nhiễm trùng và hướng dẫn s...SoM
Ã˝
Các chiến lược phân loại và điều trị viêm phổi cộng đồng 2020.pdf



Các chiến lược phân loại và điều trị viêm phổi cộng đồng 2020.pdfleonidas2507
Ã˝
More from Nguy·ªÖn H·∫°nh (15)
Cập nhật phân loại giai đoạn Ung thư bàng quang bản 8 - AJCC 2017



Cập nhật phân loại giai đoạn Ung thư bàng quang bản 8 - AJCC 2017Nguyễn Hạnh
Ã˝
Cập nhật phân loại giai đoạn Ung thư bàng quang theo TNM phiên bản 8 - AJCC 2017Cập nhật phân loại giai đoạn Ung thư phổi bản 8 - IASLC



Cập nhật phân loại giai đoạn Ung thư phổi bản 8 - IASLCNguyễn Hạnh
Ã˝
C·∫≠p nh·∫≠t ph√¢n lo·∫°i giai ƒëo·∫°n Ung th∆∞ ph·ªïi theo TNM phi√™n b·∫£n 8 - nƒÉm 2017 - IASLCCh·∫©n ƒëo√°n h√¨nh ·∫£nh ≤˙·ªán≥Û l√≠ h·ªëc m·∫Øt



Ch·∫©n ƒëo√°n h√¨nh ·∫£nh ≤˙·ªán≥Û l√≠ h·ªëc m·∫ØtNguy·ªÖn H·∫°nh
Ã˝
Ch·∫©n ƒëo√°n h√¨nh ·∫£nh ≤˙·ªán≥Û l√≠ h·ªëc m·∫ØtCH·∫®N ƒêO√ÅN H√åNH ·∫¢NH U TUY·∫æN TH∆Ø·ª¢NG ∞’±··∫¨N



CH·∫®N ƒêO√ÅN H√åNH ·∫¢NH U TUY·∫æN TH∆Ø·ª¢NG ∞’±··∫¨NNguy·ªÖn H·∫°nh
Ã˝
Chẩn đoán hình ảnh về đặc điểm u tuyến thượng thậnCập nhật chẩn đoán TIỀN SẢN GIẬT 2013



Cập nhật chẩn đoán TIỀN SẢN GIẬT 2013Nguyễn Hạnh
Ã˝
Cập nhật chẩn đoán tiền sản giậtĐiện tâm đồ trong chẩn đoán các rối loạn nhịp tim chậm



Điện tâm đồ trong chẩn đoán các rối loạn nhịp tim chậmNguyễn Hạnh
Ã˝
Chẩn đoán các rối loạn nhịp chậmCập nhật GINA 2014



C·∫≠p nh·∫≠t GINA 2014Nguy·ªÖn H·∫°nh
Ã˝
PGS TS Nguyễn Văn Đoàn
Cập nhật điều trị hen phế quản
GINA 2014Procalcitonin
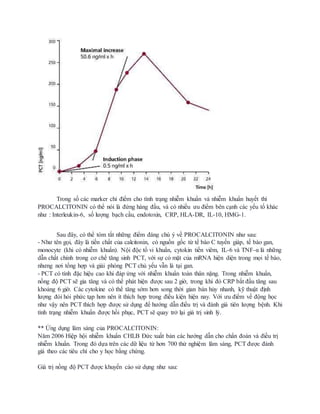
- 1. Trong s·ªë c√°c marker ch·ªâ ƒëi·ªÉm cho t√¨nh tr·∫°ng nhi·ªÖm khu·∫©n v√† nhi·ªÖm khu·∫©n huy·∫øt th√¨ PROCALCITONIN c√≥ th·ªÉ n√≥i l√† ƒë·ª©ng h√†ng ƒë·∫ßu, v√† c√≥ nhi·ªÅu ∆∞u ƒëi·ªÉm b√™n c·∫°nh c√°c y·∫øu t·ªë kh√°c nh∆∞ : Interleukin-6, s·ªë l∆∞·ª£ng b·∫°ch c·∫ßu, endotoxin, CRP, HLA-DR, IL-10, HMG-1. Sau ƒë√¢y, c√≥ th·ªÉ t√≥m t·∫Øt nh·ªØng ƒëi·ªÉm ƒë√°ng ch√∫ √Ω v·ªÅ PROCALCITONIN nh∆∞ sau: - Nh∆∞ t√™n g·ªçi, ƒë√¢y l√† ti·ªÅn ch·∫•t c·ªßa calcitonin, c√≥ ngu·ªìn g·ªëc t·ª´ t·∫ø b√†o C tuy·∫øn gi√°p, t·∫ø b√†o gan, monocyte (khi c√≥ nhi·ªÖm khu·∫©n). N·ªôi ƒë·ªôc t·ªë vi khu·∫©n, cytokin ti·ªÅn vi√™m, IL-6 v√† TNF-Œ± l√† nh·ªØng d·∫´n ch·∫•t ch√≠nh trong c∆° ch·∫ø tƒÉng sinh PCT, v·ªõi s·ª± c√≥ m·∫∑t c·ªßa mRNA hi·ªán di·ªán trong m·ªçi t·∫ø b√†o, nh∆∞ng n∆°i t·ªïng h·ª£p v√† gi·∫£i ph√≥ng PCT ch·ªß y·∫øu v·∫´n l√† t·∫°i gan. - PCT c√≥ t√≠nh ƒë·∫∑c hi·ªáu cao khi ƒë√°p ·ª©ng v·ªõi nhi·ªÖm khu·∫©n to√†n th√¢n n·∫∑ng. Trong nhi·ªÖm khu·∫©n, n·ªìng ƒë·ªô PCT s·∫Ω gia tƒÉng v√† c√≥ th·ªÉ ph√°t hi·ªán ƒë∆∞·ª£c sau 2 gi·ªù, trong khi ƒë√≥ CRP b·∫Øt ƒë·∫ßu tƒÉng sau kho·∫£ng 6 gi·ªù. C√°c cytokine c√≥ th·ªÉ tƒÉng s·ªõm h∆°n song th·ªùi gian b√°n h·ªßy nhanh, k·ªπ thu·∫≠t ƒë·ªãnh l∆∞·ª£ng ƒë√≤i h·ªèi ph·ª©c t·∫°p h∆°n n√™n √≠t th√≠ch h·ª£p trong ƒëi·ªÅu ki·ªán hi·ªán nay. V·ªõi ∆∞u ƒëi·ªÉm v·ªÅ ƒë·ªông h·ªçc nh∆∞ v·∫≠y n√™n PCT th√≠ch h·ª£p ƒë∆∞·ª£c s·ª≠ d·ª•ng ƒë·ªÉ h∆∞·ªõng d·∫´n ƒëi·ªÅu tr·ªã v√† ƒë√°nh gi√° ti√™n l∆∞·ª£ng ≤˙·ªán≥Û. Khi t√¨nh tr·∫°ng nhi·ªÖm khu·∫©n ƒë∆∞·ª£c h·ªìi ph·ª•c, PCT s·∫Ω quay tr·ªü l·∫°i gi√° tr·ªã sinh l√Ω. ** ·ª®ng d·ª•ng l√¢m s√†ng c·ªßa PROCALCITONIN: NƒÉm 2006 Hi·ªáp h·ªôi nhi·ªÖm khu·∫©n CHLB ƒê·ª©c xu·∫•t b·∫£n c√°c h∆∞·ªõng d·∫´n cho ch·∫©n ƒëo√°n v√† ƒëi·ªÅu tr·ªã nhi·ªÖm khu·∫©n. Trong ƒë√≥ d·ª±a tr√™n c√°c d·ªØ li·ªáu t·ª´ h∆°n 700 th·ª≠ nghi·ªám l√¢m s√†ng, PCT ƒë∆∞·ª£c ƒë√°nh gi√° theo c√°c ti√™u ch√≠ cho y h·ªçc b·∫±ng ch·ª©ng. Gi√° tr·ªã n·ªìng ƒë·ªô PCT ƒë∆∞·ª£c khuy·∫øn c√°o s·ª≠ d·ª•ng nh∆∞ sau:
- 2. Giá trị bình thường: PCT < 0,05 ng/ml Giá trị PCT < 0,10ng/ml: Không chỉ định dùng kháng sinh Giá trị PCT < 0,25ng/ml: Không khuyến cáo dùng kháng sinh, nếu trị liệu giảm xuống mức này thì tiếp tục dùng cho hiệu quả. Giá trị PCT > 0,25ng/ml: Khuyến cáo sử dụng kháng sinh. Giá trị PCT > 0,50 ng/ml: Chỉ định kháng sinh là bắt buộc. Giá trị PCT 0,50 - 2,0 (ng/ml): Nhiễm khuẩn do đáp ứng viêm hệ thống tương đối, nguyên nhân có thể là chấn thương, phẫu thuật sau chấn thương, sốc tim... Giá trị PCT 2,0 - 10 (ng/ml): Đáp ứng viêm hệ thống nghiêm trọng (SIRS), nguyên nhân bởi nhiễm trùng hệ thống và nhiễm khuẩn huyết, chưa có suy đa tạng. Giá trị PCT > 10 ng/ml: Đáp ứng viêm hệ thống sâu do nhiễm khuẩn huyết nghiêm trọng hoặc sốc nhiễm khuẩn. Trong nhi khoa PCT giúp chẩn đoán sớm nhiễm khuẩn xâm lấn với độ chính xác cao ( sốt <12 giờ), đặc biệt là nhiễm khuẩn toàn thân nặng de dọa mạng sống của trẻ. Ngoài ra, PCT còn được chứng minh tiên lượng được biến chứng, diễn biến của nhiễm khuẩn huyết. PCT có thể còn giúp phân biệt giữa nhiễm khuẩn huyết và SIRS, phân biệt giữa nhiễm khuẩn và thải ghép... Ngoài ra trong ứng dụng trị liệu kháng sinh dựa trên giám sát nồng độ PCT, các nhà nghiên cứu về PCT cũng khuyến cáo : Trường hợp 1: Ngừng kháng sinh nếu: a. Nồng độ PCT giảm <0,1 ng/ml Tình trạng lâm sàng cải thiện đáng kể b. Trường hợp 2:Đổi kháng sinh khác nếu: Nồng độ PCT không giảm và Triệu chứng lâm sàng tồn tại hoặc tăng thêm dấu hiệu nhiễm trùng. c. Trường hợp 3:Tiếp tục kháng sinh đang dùng nếu: Triệu chứng lâm sàng được cải thiện Nồng độ PCT không ứng với trường hợp 1 và 2. Nguồn: 1. medscape: Procalcitonin: Uses in the Clinical Laboratory for the Diagnosis of Sepsis 2. procalcitonin.com 3. Khoa khóa sinh, BV Bạch Mai Hà Nôi. 4. Bệnh viện Đa khoa MEDLATEC.










































