1 of 13
Downloaded 11 times











Recommended
第1回 ?めまい? 



第1回 ?めまい? 清水 真人
?
聖路加国際病院 救命救急センター
救急ジェネラルカンファレンス第1回「めまい」
当科を回っている研修医が作成しております。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。
更新履歴
Ver2.0 BPPVの耳石置換法を追加記載しました
Ver3.0 Take Home messageを追加記載しました
Key word
めまい, 治療, BPPV, メニエール病, 脳梗塞, 末梢性めまい, めまいの診断, めまいの治療, 救急第2回 ?一過性意识障害, 失神?



第2回 ?一過性意识障害, 失神?清水 真人
?
聖路加国際病院救命救急センター
救急ジェネラルカンファレンス第2回「一過性意识障害, 失神」
当科を回っている研修医が作成しております。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。
更新履歴
Ver2.0 心電図読影について追加記載しました第5回 ?痙攣,てんかん?



第5回 ?痙攣,てんかん?清水 真人
?
聖路加国際病院救命救急センター
救急ジェネラルカンファレンス第5回「痙攣, てんかん」
当科を回っている研修医が作成しております。このスライドは多くの文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。カフェイン中毒



カフェイン中毒清水 真人
?
カフェインは入手が容易なOTC製剤含有成分のひとつですが、時として致死的となります。その対応と臨床的特徴について簡単にまとめました。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。第4回 ?痺れ?



第4回 ?痺れ?清水 真人
?
聖路加国際病院救命救急センター
救急ジェネラルカンファレンス第4回「痺れ」
当科を回っている研修医が作成しております。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。第3回 ?頭痛?



第3回 ?頭痛?清水 真人
?
聖路加国際病院救命救急センター
救急ジェネラルカンファレンス第3回「頭痛」
当科を回っている研修医が作成しております。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。語呂で覚える 緊急気道管理



語呂で覚える 緊急気道管理清水 真人
?
▼PDFダウンロードは以下のサイトまで
https://www.igaku-seiri.com/airway/
聖路加国際病院研修医レクチャー用資料です。語呂合わせを用いることで、“安心”に“安全”で“確実”な気道管理,気管挿管を行うことを目標としています。実際の挿管テクニックや、薬剤(pretreatment, 鎮静, 筋弛緩薬)の使い方に関しては今回は割愛しています。なお、このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。なにかご不明な点がございましたら、コメントください。 第6回 ?腰背部痛?



第6回 ?腰背部痛?清水 真人
?
聖路加国際病院救命救急センター
救急ジェネラルカンファレンス第6回「腰背部痛」
当科を回っている研修医が作成しております。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。非専门医に求められる経胸壁心エコー评価について【础顿痴础狈颁贰顿】



非専门医に求められる経胸壁心エコー评価について【础顿痴础狈颁贰顿】NEURALGPNETWORK
?
by
松江生協病院
鈴木健太郎
----
5つのstepで判読する胸壁心エコー評価
① 収縮能?壁運動
②心腔径(拡大),③壁厚(肥大)
④弁機能
⑤圧の評価
⑤圧の評価(実演)
5 stepでレポートを評価する①~③
5 stepでレポートを評価する④
5 stepでレポートを評価する⑤
5 stepでレポートを評価する(①~⑤要約)
まとめ
----
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/Evernote, feedlyで簡単知識整理術!



Evernote, feedlyで簡単知識整理術!清水 真人
?
研修医向け資料です。テーマは大量の医学知識をどのように収集し整理するか。特にERにおいては「知識の引き出し」を無限に作っておく必要があります。Evernote?を使って効果的な情報整理、feedly?を使って効果的な情報収集を!4月から研修医の皆様も是非参考に、ご活用ください。
?ホームページはコチラ
?若手医師のための医学情報整理術?
https://www.igaku-seiri.com
https://www.facebook.com/igaku.seirijutsu/
?Keyword
聖路加国際病院, 救急, 医学, 医学情報整理術, 研修医, 若手医師, IT, Evernote, feedlyショック パート1 ショックのサインと诊断



ショック パート1 ショックのサインと诊断NEURALGPNETWORK
?
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/意识障害 ハ?ート2 問診、身体所見



意识障害 ハ?ート2 問診、身体所見NEURALGPNETWORK
?
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/肺塞栓症



肺塞栓症清水 真人
?
肺塞栓症のマネジメントについてです。症状の多様性と, 検査前確率の評価が難しく, 診断に難渋することがしばしばあります。各国のガイドラインを参考に概ね共通した見解を再度まとめてみました。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。不明熱?身体診察?_General Medicine Interest Group



不明熱?身体診察?_General Medicine Interest GroupKiyoshi Shikino
?
General Medicine Interest Group
千葉大学医学部医の学生が主体となり、身体診察スキルとトレーニングする学部公認のサークルです。全8回のセッションを半期で行います。興味のある方は、ご一報ください。
連絡先:千葉大学医学部附属病院 総合診療科 鋪野紀好
メール:kshikino@gmail.comめまい ハ?ート1 鑑别



めまい ハ?ート1 鑑别NEURALGPNETWORK
?
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/More Related Content
What's hot (20)
第6回 ?腰背部痛?



第6回 ?腰背部痛?清水 真人
?
聖路加国際病院救命救急センター
救急ジェネラルカンファレンス第6回「腰背部痛」
当科を回っている研修医が作成しております。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。非専门医に求められる経胸壁心エコー评価について【础顿痴础狈颁贰顿】



非専门医に求められる経胸壁心エコー评価について【础顿痴础狈颁贰顿】NEURALGPNETWORK
?
by
松江生協病院
鈴木健太郎
----
5つのstepで判読する胸壁心エコー評価
① 収縮能?壁運動
②心腔径(拡大),③壁厚(肥大)
④弁機能
⑤圧の評価
⑤圧の評価(実演)
5 stepでレポートを評価する①~③
5 stepでレポートを評価する④
5 stepでレポートを評価する⑤
5 stepでレポートを評価する(①~⑤要約)
まとめ
----
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/Evernote, feedlyで簡単知識整理術!



Evernote, feedlyで簡単知識整理術!清水 真人
?
研修医向け資料です。テーマは大量の医学知識をどのように収集し整理するか。特にERにおいては「知識の引き出し」を無限に作っておく必要があります。Evernote?を使って効果的な情報整理、feedly?を使って効果的な情報収集を!4月から研修医の皆様も是非参考に、ご活用ください。
?ホームページはコチラ
?若手医師のための医学情報整理術?
https://www.igaku-seiri.com
https://www.facebook.com/igaku.seirijutsu/
?Keyword
聖路加国際病院, 救急, 医学, 医学情報整理術, 研修医, 若手医師, IT, Evernote, feedlyショック パート1 ショックのサインと诊断



ショック パート1 ショックのサインと诊断NEURALGPNETWORK
?
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/意识障害 ハ?ート2 問診、身体所見



意识障害 ハ?ート2 問診、身体所見NEURALGPNETWORK
?
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/肺塞栓症



肺塞栓症清水 真人
?
肺塞栓症のマネジメントについてです。症状の多様性と, 検査前確率の評価が難しく, 診断に難渋することがしばしばあります。各国のガイドラインを参考に概ね共通した見解を再度まとめてみました。このスライドは文献をもとに作成しておりますが、あくまで一個人の見解であり, 病院全体の方針や意見を反映するものではありません。臨床現場へのそのままの応用は厳に慎んでください。また、スライドをお読みの方が患者?患者関係者の場合は、本内容の利用の際には必ず主治医にご相談ください。なにかご不明な点がございましたら、コメントください。不明熱?身体診察?_General Medicine Interest Group



不明熱?身体診察?_General Medicine Interest GroupKiyoshi Shikino
?
General Medicine Interest Group
千葉大学医学部医の学生が主体となり、身体診察スキルとトレーニングする学部公認のサークルです。全8回のセッションを半期で行います。興味のある方は、ご一報ください。
連絡先:千葉大学医学部附属病院 総合診療科 鋪野紀好
メール:kshikino@gmail.comめまい ハ?ート1 鑑别



めまい ハ?ート1 鑑别NEURALGPNETWORK
?
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/Viewers also liked (20)
Vasovagal syncope management Mexico City 2016



Vasovagal syncope management Mexico City 2016Antonio Raviele
?
This document discusses current management and the role of cardiac pacing in vasovagal syncope (VVS). It outlines that VVS is generally benign and self-limiting, and treatment is usually not necessary. For recurrent or high-risk cases, options discussed include non-pharmacological approaches like reassurance/counseling and counter-maneuvers, various drug therapies with limited evidence, and electrical therapies like cardiac pacing or ablation which show more promise but also have limitations and need further study. Pacing may benefit those with documented asystole, while ablation has shown reduced recurrence rates in preliminary studies but requires more research.教育講演「Fast」 のコピー



教育講演「Fast」 のコピーHirohisa Shimizu
?
This document appears to be medical records from a hospital documenting a patient's care from January 12th to 29th. It describes the patient's initial presentation with abdominal pain and distention. Imaging including CT scan revealed bleeding in the abdomen. The patient received blood transfusions and underwent an operation to stop the bleeding. Key details include a positive FAST exam, declining vital signs treated with ICU admission, and a 1 hour 44 minute long operation removing 1950ml of blood from the abdominal cavity.Vasovagal Syncope



Vasovagal SyncopeCathy Lewis
?
Vasovagal syncope (VVS) is caused by an abnormal response of the autonomic nervous system that leads to a drop in blood pressure and sometimes heart rate. It is triggered by pain, anxiety, or emotional stress and causes feelings of faintness. Those at highest risk include younger patients and those with a history of fainting. Nursing care focuses on recognizing VVS symptoms and treating lowered blood pressure and heart rate by having patients lie down with legs elevated.Approach to Syncope



Approach to SyncopeMostafa Meshaal
?
This document provides an overview of syncope (transient loss of consciousness). It defines syncope and discusses mechanisms and common causes. Cardiac causes include arrhythmias and structural heart issues. Common non-cardiac causes are neurocardiogenic syncope and orthostatic hypotension. The document outlines how to take a history and perform an exam for a syncope patient. It recommends ECG, monitoring, and risk stratification. The summary emphasizes differentiating cardiac from non-cardiac syncope, as cardiac causes have higher mortality and recommends not missing life-threatening conditions.Syncope Assessment and Management



Syncope Assessment and ManagementSCGH ED CME
?
This document contains a presentation on the assessment of syncope given to registrars at an emergency department teaching meeting. It includes two case presentations of patients who presented with syncope, along with their ECG readings, and a discussion of the differential diagnosis, evaluation algorithms, and decision rules that can be used to evaluate syncope, including the San Francisco Syncope Rule, OESIL criteria, and ROSE risk stratification. The presenter encourages questions and discussion from the audience on syncope evaluation and interesting ECG findings.Similar to 4-5.5 意识障害 (6)
地域で行う急性心不全の急性期管理について【础顿痴础狈颁贰顿】



地域で行う急性心不全の急性期管理について【础顿痴础狈颁贰顿】NEURALGPNETWORK
?
by
松江生協病院
鈴木健太郎
----
心不全へのアプローチ
? うっ血性心不全の診断
? AHF work up
?病型?病態の分類 クリニカルシナリオ(CS)
?病型?病態の分類 うっ血と低灌流
? 急性期管理~うっ血と低灌流の是正
心不全の症例① うっ血性心不全(CS4+CS3)
心不全の症例② うっ血性心不全(CS2)
心不全の症例③ うっ血性心不全(CS2)
? 心不全の原因病態への治療介入
まとめ
----
<NEURAL GP Networkとは>
島根県初?総合診療医育成プロジェクト
地域医療現場と大学を結ぶTeal型組織構造
診療医療の育成は現場においてのみ可能である。
しかし、現場だけでは日本全体の総合診療を成長させるには不十分。
だから、わたしたちは今、
島根県からITを駆使して総合医療のニューラルネットワーク構築を目指します。
NEURAL GP Network WEBサイト: https://shimanegp.com/
More from Kenji Kawanai (20)
妊娠自覚のない妊娠36週未受诊妊妇が急性腹症で救急要请したが、子宫内胎児死亡および死产と判明した1例



妊娠自覚のない妊娠36週未受诊妊妇が急性腹症で救急要请したが、子宫内胎児死亡および死产と判明した1例Kenji Kawanai
?
妊娠自覚のない妊娠36週未受诊妊妇が急性腹症で救急要请したが、子宫内胎児死亡および死产と判明した1例
腸閉塞により妊娠29週に緊急帝王切開術および癒着剥離術を施行したものの, 再度腸閉塞を発症し腸管切除に至った1例



腸閉塞により妊娠29週に緊急帝王切開術および癒着剥離術を施行したものの, 再度腸閉塞を発症し腸管切除に至った1例Kenji Kawanai
?
腸閉塞により妊娠29週に緊急帝王切開術および癒着剥離術を施行したものの, 再度腸閉塞を発症し腸管切除に至った1例
自闭症



自闭症Kenji Kawanai
?
スーパー コピペ
自閉傾向
アスペルガー 微々傾向ある僕として
示唆に富んでいたのは
社会的不行動←「混乱が 本質」なのであるから
対策必須
→入力 減
入力 simple
→小さいフローをちゃんと回すこと4-5.5 意识障害
- 1. 意识障害 unit 4 :循環器- ⑤ case:「胸が痛い倒れる」 大動脈解離→?心タンポナーデ?AR →脈左右差意識消失 参考文献: 病気が見える脳?神経 わかりやすい内科学文光堂 意识障害のある患者の理解と看護中山書店 昏睡と意识障害メディカル?サイエンス?インターナショナル他 2014 10/3 Group 9 08211011 河内健二
- 2. 今回全体の流れ ? 高血圧喫煙歴65歳 →大動脈解離stanfordA →腕頭動脈虚血(分枝虚血) →内頚動脈虚血 + →… →心タンポナーデ →心拍出低下 (→出血性ショック) →脳虚血 →上位脳幹網様体障害 →意識消失 救急車到着時JCS Ⅲー200 →救急車処置 →病院到着時Ⅱー30 瞳孔OK 対光反射OK (=視床下部以下?の脳の神経自体は器質的に異常なし) →病院処置→Ⅱー20 若干の左半身不全麻痺残存 →心タンポナーデ解除手術 →脳血流循環量回復 →意識レベル完全に回復 疑問:今回は大動脈解離心タンポナーデだが 具体的に何の処置が経過中なされたのだろう? 心臓マッサージってやっていいの?
- 3. 意识障害:目次 ? 意識とは 意識の3要素 構造意識中枢 ? 意识障害 分類 ? 診断の進め方 評価スケール ? 治療 緊急 慢性
- 4. 意識とは (意識の3要素) (「覚醒と自己と外界環境の認識」) ①覚醒度: まずonになってるか通じてるか 有るか無しか →賦活系 ②広がり: →大脳皮質全体前頭葉で統合 ③質:
- 5. 意識中枢さらっと 意識←構造 ? 大脳皮質: 意識の座自体 神経細胞のほにゃらら→意識機能を成り立たせてる ? 大脳辺縁系 ? ←視床(間脳) (視床下部賦活系) ?←脳幹網様体上行性網様体賦活系 ? ←末梢からの感覚入力
- 6. 意识障害分類 3要素それぞれに対応 ①意識混濁←覚醒度 混濁か晴明か ②意識狭窄←広がり 認知?判断?思考?心理? などの機能低下により一つの対象だけに注意が集中 もしくは連想想像などができない ③意識変容:異常精神活動 (幻覚?錯覚?興奮?不安)
- 7. 意识障害の原因 感覚刺激入力→…→…→大脳皮質神経細胞ネットワーク→意識機能成立 「どこかの段階の神経細胞が何らかの原因で機能しなくなるか ら」(細かい細胞以下の機序の話は不明であります!) ←①中枢神経系自体への直接ダメージいわゆる器質的 ②全身疾患で神経系もダウン二次的 ③心因性に自爆転換反応 AIUEO TIPS で網羅!
- 8. 意识障害の原因 ? A アルコール ? I 低血糖insulin ? U 尿毒症uremia ? E 脳症encephalopathy / 内分泌疾患endocrin 電解質異常electrolytes 不整脈electrocardiogram てんかんepilepsy ? O 低酸素血症薬物中毒overdose ? T 頭部外傷trauma /高体温低体温temperature ? I 感染症infection ? P 精神疾患psychiatric ポルフィリア ? S 脳血管障害stroke 痙攣重積seizure ? / 失神syncope ショックshock
- 9. 診断の進め方 ? 病態把握 スケールと刺激反応(試験)利用 →鑑別疾患どこに病変が存在するか ? GCSスケールをつかえば→ 除皮質硬直?除脳硬直 ?眼球運動?嚥下有無まで調べると→ 閉じ込め症候群 無動性無言 失外套症候群鑑別できる!!!
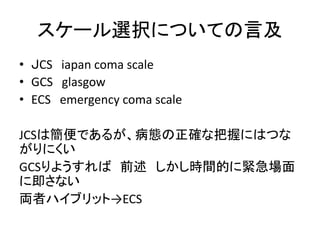
- 10. スケール選択についての言及 ? JCS iapan coma scale ? GCS glasgow ? ECS emergency coma scale JCSは簡便であるが、病態の正確な把握にはつな がりにくい GCSりようすれば前述しかし時間的に緊急場面 に即さない 両者ハイブリット→ECS
- 11. 診断の進め方 ポイント①責任病巣病変部位はどこか? ②意识障害の原因(となった病態)は何か? スケール利用+ バイタルサイン 神経学的検査→大脳なのか脳幹なのか 病歴→OPQRST 血液検査→代謝疾患動脈血酸素分圧毒物 心電図→心原性 画像検査頭部CT→外傷出血性病変 髄駅検査→炎症性疾患 脳波→てんかん確定診断
- 12. 治療急性 BLS 一次救命処置basic life support ALS 二次救命処置advanced ①呼吸の確認呼吸の確保 ②循環の確保→今回は大動脈解離心タンポナーデだが 具体的に何の処置が経過中なされたのだろう? AIUEO TIPS それぞれ ③ブドウ糖投与 ④体温調節 ⑤頭蓋内圧下げる ⑥痙攣を止める ⑦電解質ph の補正 ⑧拮抗薬の投与
- 13. 治療というかケア看護 慢性的意识障害昏睡(植物状態)に対して 植物状態:(昏睡状態の)慢性ver で呼吸と循環は維持されている 睡眠覚醒周期をもつ? 網様体賦活系は現存大脳機能停止脳幹機能残存 ? 排尿管理 ? 排便補助 ? 清潔(全身陰部口腔) ? 栄養補給経静脈栄養 経(消化)管栄養経鼻経腸 ?褥瘡?関節拘縮予防


















































